
Get the free Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, D...
Show details
This document outlines the coverage determination for Erythropoiesis Stimulating Agents used in treating anemia, specifically focusing on Epoetin alfa, Darbepoetin alfa, and Peginesatide. It addresses
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign local coverage determination for
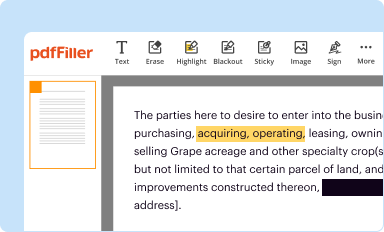
Edit your local coverage determination for form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
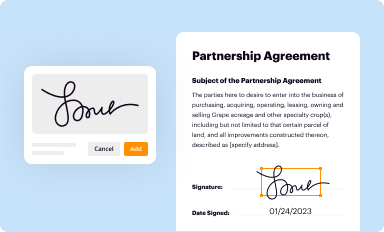
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your local coverage determination for form via URL. You can also download, print, or export forms to your preferred cloud storage service.
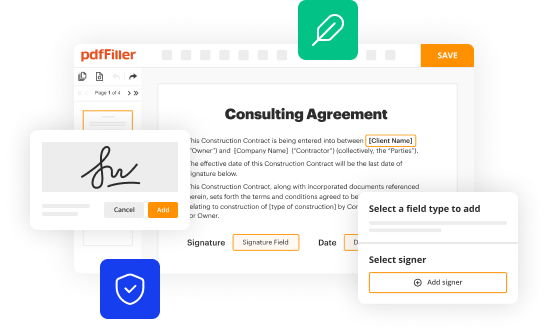
How to edit local coverage determination for online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Log in to your account. Click on Start Free Trial and sign up a profile if you don't have one.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit local coverage determination for. Text may be added and replaced, new objects can be included, pages can be rearranged, watermarks and page numbers can be added, and so on. When you're done editing, click Done and then go to the Documents tab to combine, divide, lock, or unlock the file.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
It's easier to work with documents with pdfFiller than you could have believed. You can sign up for an account to see for yourself.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out local coverage determination for
How to fill out Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide
01
Begin by reviewing the specific Local Coverage Determination (LCD) guidelines for Erythropoiesis Stimulating Agents (ESAs) to ensure compliance.
02
Gather patient information, including medical history, diagnosis, and treatment plans relevant to the use of Epoetin alfa, Darbepoetin alfa, or Peginesatide.
03
Document laboratory values such as hemoglobin levels and related blood tests to support the medical necessity of the ESA.
04
Provide detailed clinical rationale for the use of the ESA, including previous treatments and their outcomes.
05
Include documentation of patient eligibility based on the FDA-approved indications for the specific ESA being prescribed.
06
Clearly annotate the dosage and administration schedule proposed for the chosen ESA.
07
Ensure all information is organized according to the format required by the payer, following any specific instructions provided in the LCD.
08
Submit the completed LCD request along with any necessary supporting documentation and follow up as needed.
Who needs Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
01
Patients with chronic kidney disease who require anemia management.
02
Individuals undergoing chemotherapy who are experiencing anemia related to cancer treatments.
03
Patients with certain types of anemia related to autoimmune conditions or other underlying health issues.
04
Individuals needing preoperative anemia management to reduce the risk of blood transfusions.
Fill
form
: Try Risk Free






People Also Ask about
What are erythropoiesis-stimulating agents epoetin alfa?
Epoetin injection is used to treat anemia in patients with chronic kidney disease (CKD) who may or may not be on dialysis. This medicine may also be used to prevent or treat anemia that is caused by surgery or medicines (eg, zidovudine) that are used for other conditions, such as HIV or cancer.
Does Medicare cover epoetin alfa?
Epogen is also available as a biosimilar. Biosimilars are biologic drugs that are similar to the original medication with no meaningful differences in effectiveness or safety. The currently approved biosimliar for epogen is retacrit (epoetin alfa-epbx). Epogen may be covered by your Medicare or insurance plan.
When is retacrit indicated?
RETACRIT is indicated for the treatment of anemia due to chronic kidney disease (CKD), including patients on dialysis and not on dialysis to decrease the need for red blood cell (RBC) transfusion.
What is the difference between darbepoetin alfa and epoetin alfa?
In comparison to epoetin alfa, darbepoetin alfa (DPO) contains an increased amount of sialic acid-containing carbohydrate chains. It shows a much longer elimination half-life than epoetin alfa, with prolonged erythropoietic effect.
What is the alternative to retacrit?
Retacrit Alternatives Compared Retacrit (epoetin alfa)Reblozyl (luspatercept)Epoetin alfa Dosage Forms Injectable solution Subcutaneous powder for injection N/A Brand Names Other epoetin alfa brands include: Epogen, Procrit N/A Epogen, Procrit, Retacrit39 more rows
What is the protocol for retacrit?
The recommended RETACRIT regimens are: 300 Units/kg per day subcutaneously for 15 days total: administered daily for 10 days before surgery, on the day of surgery, and for 4 days after surgery.
Is retacrit expensive?
The active ingredient in this medication is epoetin alfa. It is available in the form of an injectable solution and is not covered by Medicare. There is currently no generic alternative available. The average retail price of 1, 1ML of 40000UNIT/ML vial of Retacrit is typically around $529.99.
What is the difference between Procrit and Retacrit?
RETACRIT is an FDA-approved biosimilar* to Epogen®/Procrit® (epoetin alfa). This means there are no clinically meaningful differences in terms of safety, purity, or potency (safety and effectiveness). That is, RETACRIT is expected to work in the same way.
What are the two main reasons why Epogen is prescribed?
USES: This medication is used to treat anemia (low red blood cell count) in people with long-term serious kidney disease (chronic kidney failure), people receiving zidovudine to treat HIV, and people receiving chemotherapy for some types of cancer (cancer that does not involve the bone marrow or blood cells).
Is retacrit a medical necessity?
Therefore, Aetna considers Epogen, Mircera, and Retacrit to be medically necessary only for members who have a contraindication, intolerance or ineffective response to the available equivalent alternatives Aranesp and Procrit.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
Local Coverage Determination (LCD) for Erythropoiesis Stimulating Agents (ESAs) like Epoetin alfa, Darbepoetin alfa, and Peginesatide outlines the criteria and guidelines under which Medicare will reimburse for the use of these medications, primarily for treating anemia related to chronic kidney disease or chemotherapy.
Who is required to file Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
Healthcare providers or facilities that wish to receive reimbursement from Medicare for administering ESAs must comply with the Local Coverage Determination guidelines and provide necessary documentation as specified.
How to fill out Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
To fill out the Local Coverage Determination, providers should follow the guidelines by collecting necessary patient data, documenting clinical indications for ESA use, ensuring the documentation meets LCD criteria, and submitting the forms to the appropriate Medicare Administrative Contractor.
What is the purpose of Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
The purpose of the Local Coverage Determination is to define the circumstances under which Erythropoiesis Stimulating Agents are medically necessary, thus ensuring appropriate use of these agents and preventing unnecessary expenditures by Medicare.
What information must be reported on Local Coverage Determination for Erythropoiesis Stimulating Agents - Epoetin alfa, Darbepoetin alfa, Peginesatide?
The information that must be reported includes patient medical history, laboratory results indicating anemia, prescribed dosages, treatment duration, and any other relevant clinical information that supports the necessity for ESA therapy according to the LCD.
Fill out your local coverage determination for online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Local Coverage Determination For is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.





















