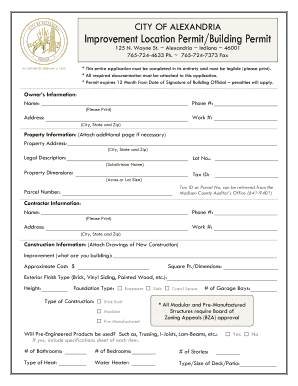
Get the free Documentation Guidelines - Physical Therapists
Show details
This document provides detailed guidelines for physical therapists on the necessary documentation standards required by Blue Cross and Blue Shield of Kansas (BCBSKS) for proper reimbursement of services.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign documentation guidelines - physical
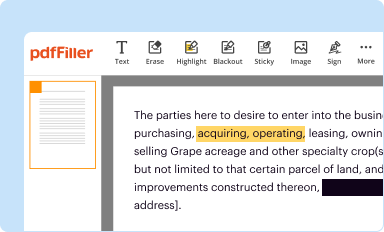
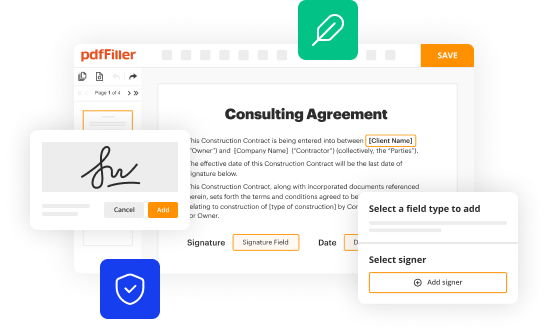
Edit your documentation guidelines - physical form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
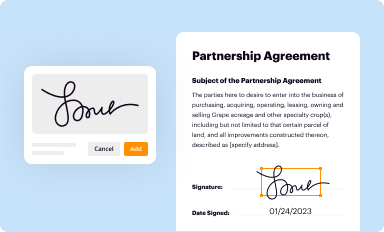
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
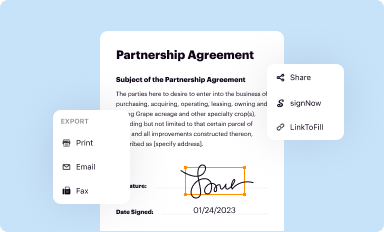
Share your form instantly
Email, fax, or share your documentation guidelines - physical form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit documentation guidelines - physical online
To use our professional PDF editor, follow these steps:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit documentation guidelines - physical. Replace text, adding objects, rearranging pages, and more. Then select the Documents tab to combine, divide, lock or unlock the file.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
With pdfFiller, dealing with documents is always straightforward.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out documentation guidelines - physical
How to fill out Documentation Guidelines - Physical Therapists
01
Begin by reviewing the purpose of the documentation guidelines.
02
Gather all necessary patient information and medical history.
03
Document the initial evaluation, including patient goals and assessment.
04
Record treatment plans, specifying techniques, frequencies, and expected outcomes.
05
Note progress regularly, including any modifications to the treatment plan.
06
Ensure all entries are clear, concise, and use appropriate medical terminology.
07
Include patient consent forms and any relevant communication with other healthcare providers.
08
Review the documentation for completeness and accuracy before finalizing.
Who needs Documentation Guidelines - Physical Therapists?
01
Physical therapists practicing in clinics, hospitals, or private settings.
02
Healthcare administrators overseeing physical therapy departments.
03
Insurance providers requiring documentation for claims processing.
04
Students and new graduates seeking to understand professional standards.
05
Regulatory bodies monitoring compliance with healthcare documentation standards.
Fill
form
: Try Risk Free






People Also Ask about
Which of the following is included in rehabilitative therapy documentation?
Documentation of each treatment note must include the following required elements: Date of treatment. Identification of each specific intervention/modality provided and billed (both timed and untimed codes). Total timed code treatment minutes and total treatment time in minutes.
What is required in physical therapy documentation?
Though your physical therapy documentation may expand as a patient continues along an episode of care, general components of quality physical therapy documentation examples include: Patient details (DOB, name, physician contact information) Medical diagnosis. Past medical and PT treatment history.
What is the APTA discharge summary?
The purpose of the discharge document is to summarize a patient's/client's progress toward goals, status at discharge, and future plans for self-management. Essentially, as the APTA puts it, it is “the last opportunity a therapist has to convey the outcome of physical therapy services.
Who is directly responsible for ensuring appropriate documentation for all physical therapy services?
A physical therapist shall assess and document patient status and any change in the program being provided by a physical therapist assistant on a timely basis.
What are the requirements for physical therapy documentation?
Complete physical therapy documentation should include important patient details such as age and date of birth, the patient's medical diagnosis and any relevant medical history, any medications and dosages, a physical therapy assessment and diagnosis, physical therapy goals and plan of care, and appropriate CPT billing
What are the requirements for a progress note in physical therapy?
The Progress Report At minimum, a licensed therapist must complete a progress note—a.k.a. progress report—for every patient by his or her tenth visit. In it, the therapist must: Include an evaluation of the patient's progress toward current goals. Make a professional judgment about continued care.
What is a clinical practice guideline for physical therapy?
Clinical Practice Guidelines (CPG) are graded recommendations on best practice for a specific condition based on the systematic review and evaluation of the quality of the scientific literature.
How to document PT?
Physical Therapy Documentation Requirements [ ] Patient details (DOB, name, physician contact information) [ ] Medical diagnosis. [ ] Past medical and PT treatment history. [ ] Medication history. [ ] Physical therapy assessment and diagnosis. [ ] Physical therapy treatment goals and plan of care. [ ] Billing CPT codes.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Documentation Guidelines - Physical Therapists?
Documentation Guidelines for Physical Therapists outlines the standards and best practices for documenting patient care and treatment in compliance with legal and regulatory requirements.
Who is required to file Documentation Guidelines - Physical Therapists?
All licensed physical therapists and physical therapist assistants who provide services must adhere to these documentation guidelines as part of their professional responsibilities.
How to fill out Documentation Guidelines - Physical Therapists?
To fill out the guidelines, therapists must accurately record patient evaluations, treatment plans, progress notes, and discharge summaries while ensuring that all required information is complete and clear.
What is the purpose of Documentation Guidelines - Physical Therapists?
The purpose of the guidelines is to ensure consistent and accurate documentation, facilitate communication among healthcare providers, support reimbursement processes, and maintain legal protection for both therapists and patients.
What information must be reported on Documentation Guidelines - Physical Therapists?
Key information includes patient demographics, clinical findings, treatment goals, interventions provided, patient progress, and any changes to treatment plans.
Fill out your documentation guidelines - physical online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Documentation Guidelines - Physical is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.