PA Aetna Better Health PA-15-06-01 2021-2025 free printable template
Show details
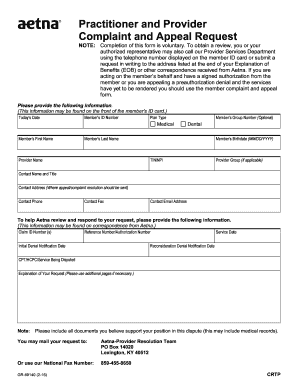
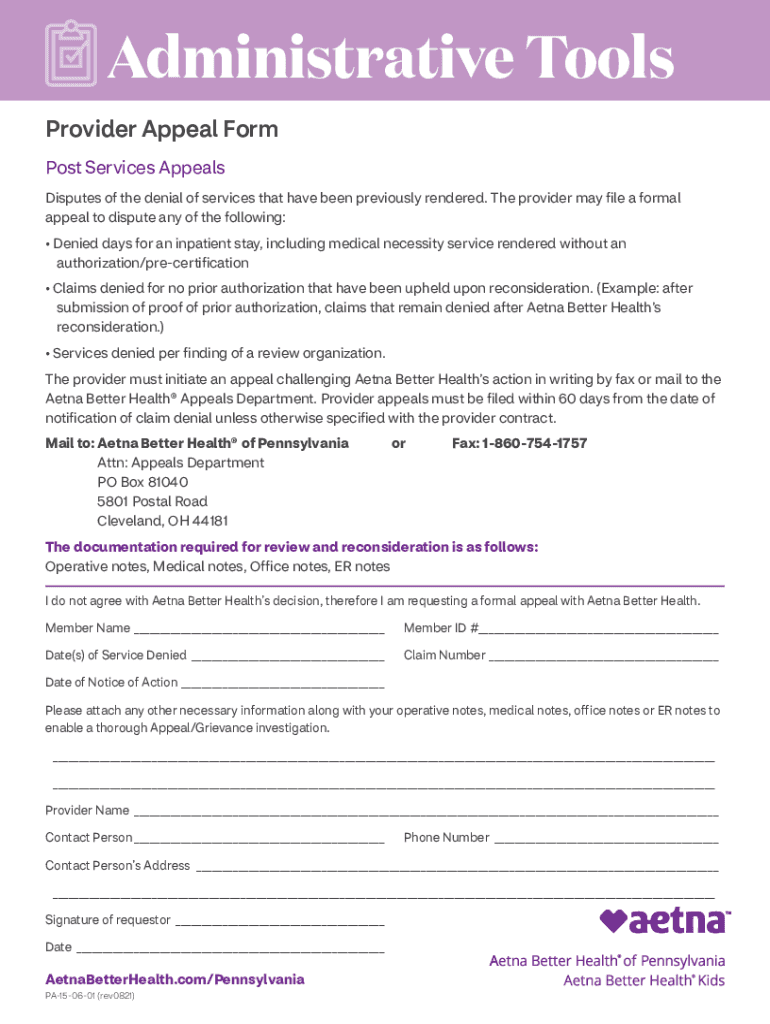
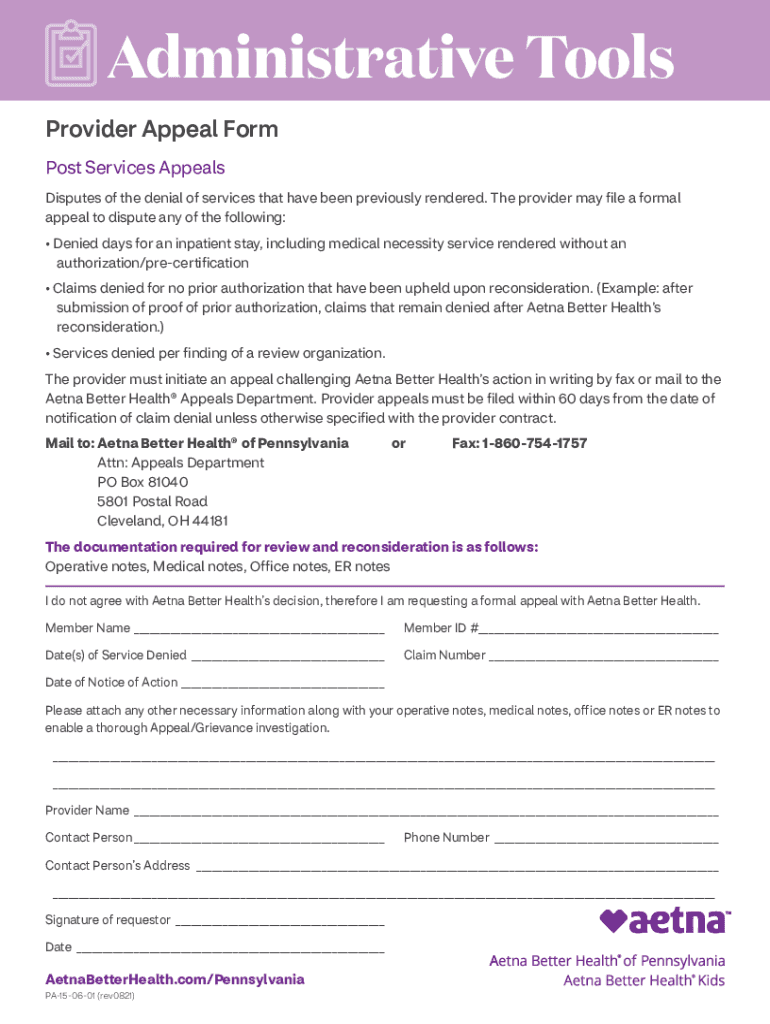
Administrative Tools Provider Appeal Form Post Services Appeals Disputes of the denial of services that have been previously rendered. The provider may file a formal appeal to dispute any of the following:
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign aetna better health pa form
Edit your aetna provider appeal form pdf form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
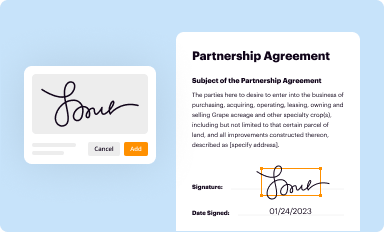
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
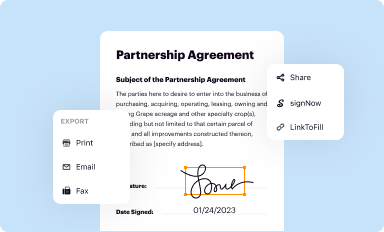
Share your form instantly
Email, fax, or share your aetna better health pennsylvania form via URL. You can also download, print, or export forms to your preferred cloud storage service.
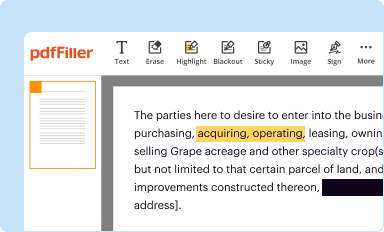
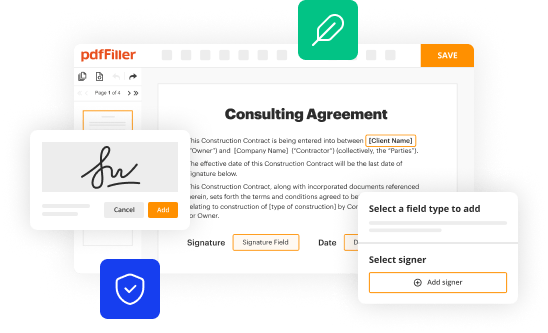
Editing aetna better health pa form online
To use our professional PDF editor, follow these steps:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Simply add a document. Select Add New from your Dashboard and import a file into the system by uploading it from your device or importing it via the cloud, online, or internal mail. Then click Begin editing.
3
Edit aetna better health of pennsylvania form. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Save your file. Select it from your list of records. Then, move your cursor to the right toolbar and choose one of the exporting options. You can save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud, among other things.
It's easier to work with documents with pdfFiller than you could have believed. You can sign up for an account to see for yourself.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
PA Aetna Better Health PA-15-06-01 Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out PA Aetna Better Health PA-15-06-01
How to fill out provider disputes and appealsohiomedicare
01
Start by obtaining a copy of the Medicare Summary Notice (MSN) or Explanation of Benefits (EOB) that details the claim you are disputing.
02
Contact the provider's office or the Medicare claims department to discuss the issue and try to resolve it informally.
03
If the issue is not resolved, you can submit a formal written appeal to Medicare within 120 days of receiving the MSN or EOB.
04
Include specific reasons for the dispute, any supporting documentation or evidence, and your Medicare number on the appeal form.
05
Wait for a response from Medicare, which will review the appeal and make a decision based on the evidence provided.
Who needs provider disputes and appealsohiomedicare?
01
Individuals who have received a Medicare Summary Notice or Explanation of Benefits and believe there is an error in the billing or coverage.
02
Healthcare providers or facilities that are disputing a claim denial or reimbursement amount from Medicare.
Fill
form
: Try Risk Free






People Also Ask about
What is timely filing limit in healthcare?
Health insurance companies have their guidelines, and usually, the timely filing limit ranges from 30 days to 1 year from the day of service. You can find timely filing limits under the claims section in the provider manual. The insurers are not responsible for late claims.
Does every insurance has same timely filing limit?
But is there any time limit for filing such claims? The answer to this is 'No'. However, insurers will check whether the policy was active at the time of the event .
Why is Aetna denying my claim?
The most common reasons for denials from health insurance providers like Aetna include: Your doctor provided insufficient evidence of medical necessity. You failed to use an in-network provider.
What does dispute claim mean?
Disputed Claim means that portion (including, when appropriate, the whole) of a Claim that is not an Allowed Claim or is subject to an Estimation Request, or as to which an objection has been filed.
What is a dispute in assessment?
Student disagrees with an assessment decision. Student examines the standards/criteria and still feels the assessment decision is wrong/unfair.
What is Aetna's timely filing limit?
We've changed the standard nonparticipating-provider timely filing limit from 27 months to 12 months for traditional medical claims. The updated limit will: Start on January 1, 2022. Maintain dental limits at 27 months.
What is dispute claim?
Disputed Claim means that portion (including, when appropriate, the whole) of a Claim that is not an Allowed Claim or is subject to an Estimation Request, or as to which an objection has been filed.
What is the difference between dispute and appeal?
An appeal often comes after a legal dispute has been resolved. If one of the parties believes that the judge, juries, or lawyers made a mistake that resulted in the wrong court results, they can file an appeal.
What is a dispute example?
an argument or disagreement, especially an official one between, for example, workers and employers or two countries with a common border: a bitter/long-running dispute. a border dispute. a pay/legal/trade dispute. They have been unable to settle/resolve the dispute over working conditions.
What happens when Aetna denies a claim?
If your claim is denied, we will send you a letter to let you know. If you don't agree, you can file an appeal. Once there are no appeals left, independent doctors may review your denied claim. This is called an external review.
How does a claim become a dispute?
Disputes become claims when the contractor lists them as exceptions to the proposed final estimate. within the time specified. Make every effort to provide a complete response to the contractor's request. If it is unclear about what is being requested, ask the contractor to clarify the request.
How do I appeal an Aetna denial?
You or your doctor may ask for an "expedited" appeal. Call the toll-free number on your Member ID card or the number on the claim denial letter. If your plan has one level of appeal, we'll tell you our decision no later than 72 hours after we get your request for review.
Why is Aetna denying claims?
The most common reasons for denials from health insurance providers like Aetna include: Your doctor provided insufficient evidence of medical necessity. You failed to use an in-network provider. You failed to obtain prior authorization or pre-certification for your service or treatment.
What is the timely filing limit?
Denials for “Timely Filing” In medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year.
What is the TFL for Aetna?
Timely Filing Requirements of Claims New claims must be submitted within 180 calendar days from the date of service. Claims will deny if not received within the required time frames. Corrected claims must be submitted within 365 days from the date of service.
How do I appeal an insurance decision?
To appeal the denial, you should take the following steps within 30 days of receiving the denial letter from your insurer: Review the determination letter. Collect information. Request documents. Call your health care provider's office. Submit the appeal request. Request an expedited internal appeal, if applicable.
What is the difference between a dispute and appeal?
What Is an Appeal? An appeal often comes after a legal dispute has been resolved. If one of the parties believes that the judge, juries, or lawyers made a mistake that resulted in the wrong court results, they can file an appeal.
How do I appeal a no authorization denial?
You or your doctor contact your insurance company and request that they reconsider the denial. Your doctor may also request to speak with the medical reviewer of the insurance plan as part of a “peer-to-peer insurance review” in order to challenge the decision.
What happens when you dispute a claim?
Once filed, your dispute is then turned over to the bank or card network for investigation. Your bank will typically give you a provisional refund, which will be in place until your claim can be validated by the bank.
What is the difference of appeal?
An appeal is not another trial. Instead, it is a review of the original decision entered by the lower level court. That means that appeals decisions cannot be made based on new factors, although an appellate court can sometimes decide that the trial court failed to consider critical evidence.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send PA Aetna Better Health PA-15-06-01 to be eSigned by others?
Once your PA Aetna Better Health PA-15-06-01 is ready, you can securely share it with recipients and collect eSignatures in a few clicks with pdfFiller. You can send a PDF by email, text message, fax, USPS mail, or notarize it online - right from your account. Create an account now and try it yourself.
Can I sign the PA Aetna Better Health PA-15-06-01 electronically in Chrome?
Yes, you can. With pdfFiller, you not only get a feature-rich PDF editor and fillable form builder but a powerful e-signature solution that you can add directly to your Chrome browser. Using our extension, you can create your legally-binding eSignature by typing, drawing, or capturing a photo of your signature using your webcam. Choose whichever method you prefer and eSign your PA Aetna Better Health PA-15-06-01 in minutes.
How do I complete PA Aetna Better Health PA-15-06-01 on an Android device?
Complete your PA Aetna Better Health PA-15-06-01 and other papers on your Android device by using the pdfFiller mobile app. The program includes all of the necessary document management tools, such as editing content, eSigning, annotating, sharing files, and so on. You will be able to view your papers at any time as long as you have an internet connection.
What is provider disputes and appealsohiomedicare?
Provider disputes and appeals ohiomedicare is the process through which healthcare providers can challenge decisions made by Medicare regarding reimbursement or coverage of services.
Who is required to file provider disputes and appealsohiomedicare?
Healthcare providers who disagree with a decision made by Medicare regarding reimbursement or coverage of services are required to file provider disputes and appeals ohiomedicare.
How to fill out provider disputes and appealsohiomedicare?
Providers can fill out provider disputes and appeals ohiomedicare by completing the necessary forms and submitting supporting documentation to Medicare.
What is the purpose of provider disputes and appealsohiomedicare?
The purpose of provider disputes and appeals ohiomedicare is to give healthcare providers an opportunity to challenge Medicare's decisions and potentially reverse them.
What information must be reported on provider disputes and appealsohiomedicare?
Providers must report details of the dispute, supporting documentation, and any other relevant information on provider disputes and appeals ohiomedicare.
Fill out your PA Aetna Better Health PA-15-06-01 online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
PA Aetna Better Health PA-15-06-01 is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.