Get the free Claim denials related to TPL amount is less than % specified
Show details
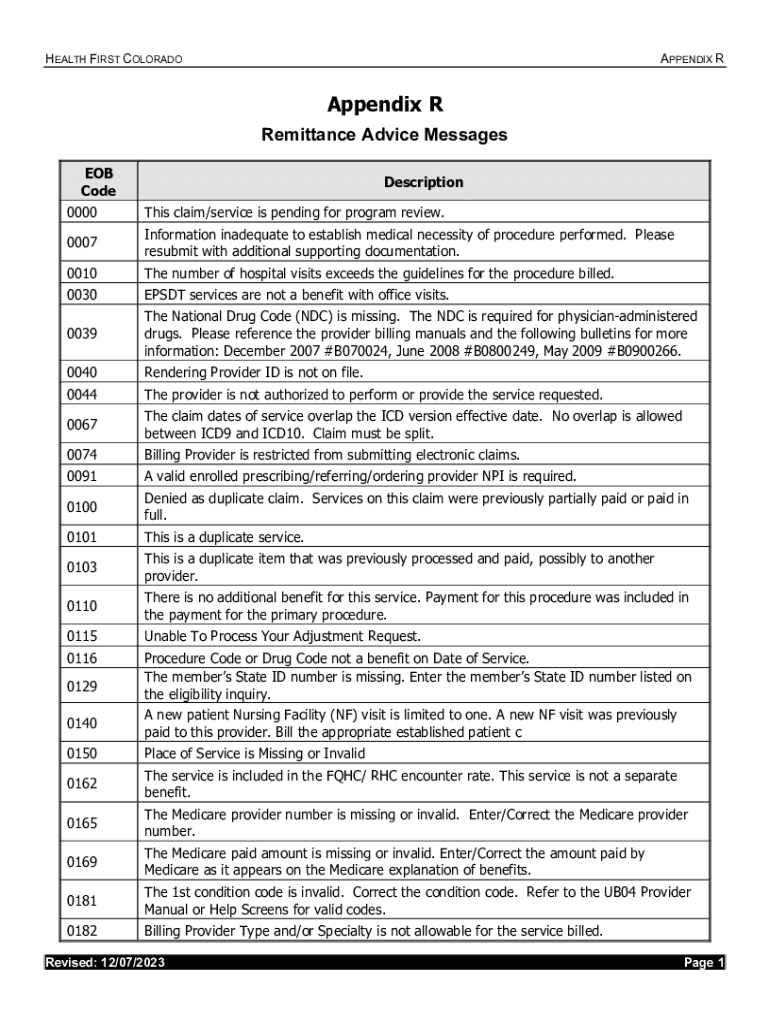
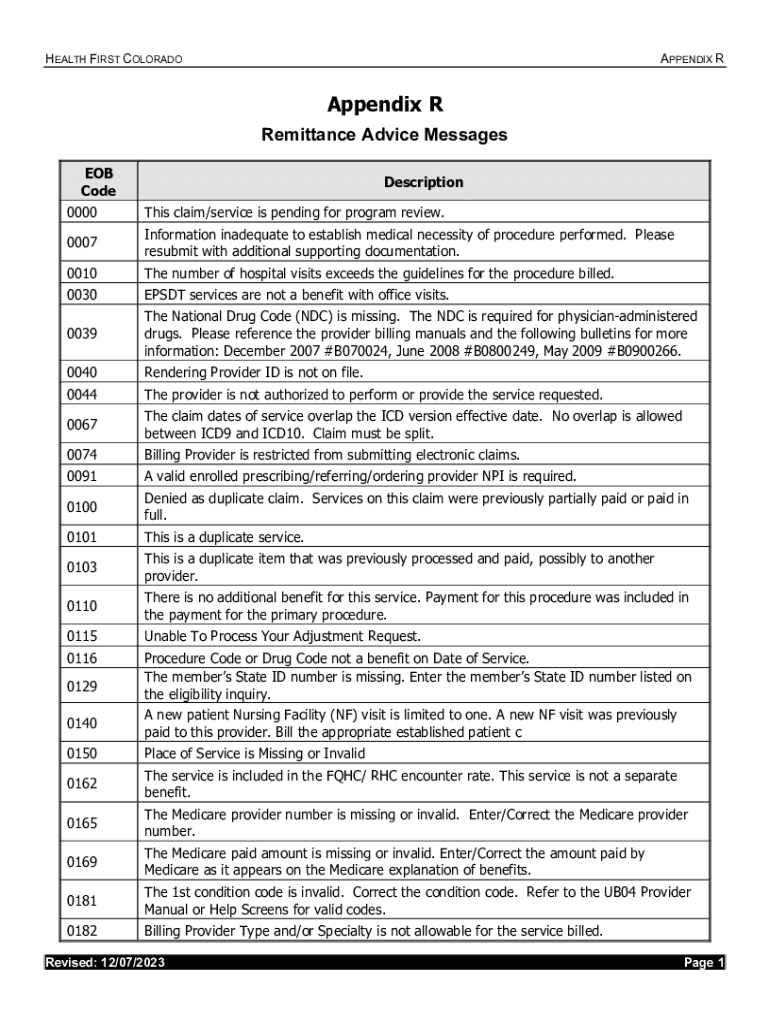
HEALTH FIRST COLORADOAPPENDIX RAppendix R Remittance Advice Messages EOB CodeDescription0000This claim/service is pending for program review.0007Information inadequate to establish medical necessity
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign claim denials related to
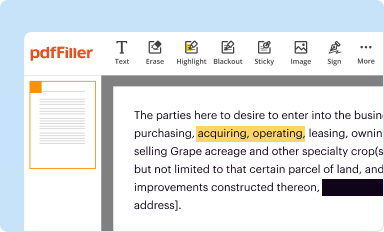
Edit your claim denials related to form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your claim denials related to form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing claim denials related to online
Follow the guidelines below to benefit from a competent PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Upload a document. Select Add New on your Dashboard and transfer a file into the system in one of the following ways: by uploading it from your device or importing from the cloud, web, or internal mail. Then, click Start editing.
3
Edit claim denials related to. Rearrange and rotate pages, add and edit text, and use additional tools. To save changes and return to your Dashboard, click Done. The Documents tab allows you to merge, divide, lock, or unlock files.
4
Save your file. Select it in the list of your records. Then, move the cursor to the right toolbar and choose one of the available exporting methods: save it in multiple formats, download it as a PDF, send it by email, or store it in the cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out claim denials related to
How to fill out claim denials related to
01
Gather all the necessary information related to the claim denial, including claim number, date of service, and denial reason.
02
Review the denial reason and understand the specific issue or requirement that needs to be addressed.
03
Prepare a letter or a form to submit the claim denial appeal, addressing it to the appropriate department or individual.
04
Clearly state the reason for the appeal and provide any supporting documentation or evidence to justify the claim.
05
Ensure that the appeal includes complete and accurate information, including patient details, provider details, and service details.
06
Submit the claim denial appeal within the specified timeframe, following any specific instructions provided by the insurance company or organization.
07
Keep a copy of the appeal submission for your records and request confirmation of receipt if possible.
08
Monitor the progress of the appeal and follow up with the insurance company or organization if needed.
09
Be prepared for additional requests for information or clarification, and provide timely responses to ensure the appeal process proceeds smoothly.
10
Document all communication related to the claim denial appeal, including dates, names, and details of conversations or correspondence.
11
If the claim denial appeal is successful, ensure that the claim is properly processed and any payment or adjustment is received.
12
If the claim denial appeal is unsuccessful, consider seeking further assistance or exploring other options, such as involving a healthcare advocate or filing a complaint.
Who needs claim denials related to?
01
Anyone who has had a claim denied by an insurance company or healthcare organization.
02
Healthcare providers who want to challenge claim denials on behalf of their patients.
03
Patients who believe their claim was incorrectly denied or not properly processed.
04
Individuals responsible for the administration and management of healthcare claims, such as medical billing professionals or insurance claims processors.
Fill
form
: Try Risk Free






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send claim denials related to to be eSigned by others?
When you're ready to share your claim denials related to, you can swiftly email it to others and receive the eSigned document back. You may send your PDF through email, fax, text message, or USPS mail, or you can notarize it online. All of this may be done without ever leaving your account.
How do I edit claim denials related to in Chrome?
Get and add pdfFiller Google Chrome Extension to your browser to edit, fill out and eSign your claim denials related to, which you can open in the editor directly from a Google search page in just one click. Execute your fillable documents from any internet-connected device without leaving Chrome.
How do I fill out claim denials related to using my mobile device?
You can quickly make and fill out legal forms with the help of the pdfFiller app on your phone. Complete and sign claim denials related to and other documents on your mobile device using the application. If you want to learn more about how the PDF editor works, go to pdfFiller.com.
What is claim denials related to?
Claim denials are related to the refusal by a payer to reimburse a healthcare provider for services rendered to a patient due to various reasons such as incorrect information, lack of medical necessity, or failure to meet policy requirements.
Who is required to file claim denials related to?
Healthcare providers, including hospitals and doctors, are required to file claim denials related to the claims they submit for reimbursement when they believe the denials were improper or unjustified.
How to fill out claim denials related to?
To fill out claim denials, providers need to include details such as patient information, claim number, specific reason for denial, supporting documents, and any additional information necessary for the appeals process.
What is the purpose of claim denials related to?
The purpose of claim denials is to ensure that claims submitted for reimbursement adhere to payer regulations, provide an opportunity for providers to appeal incorrect denials, and ultimately ensure appropriate compensation for healthcare services.
What information must be reported on claim denials related to?
Information that must be reported on claim denials includes the claim number, patient demographics, dates of service, reasons for denial, and any relevant documentation that supports the appeal.
Fill out your claim denials related to online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Claim Denials Related To is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.