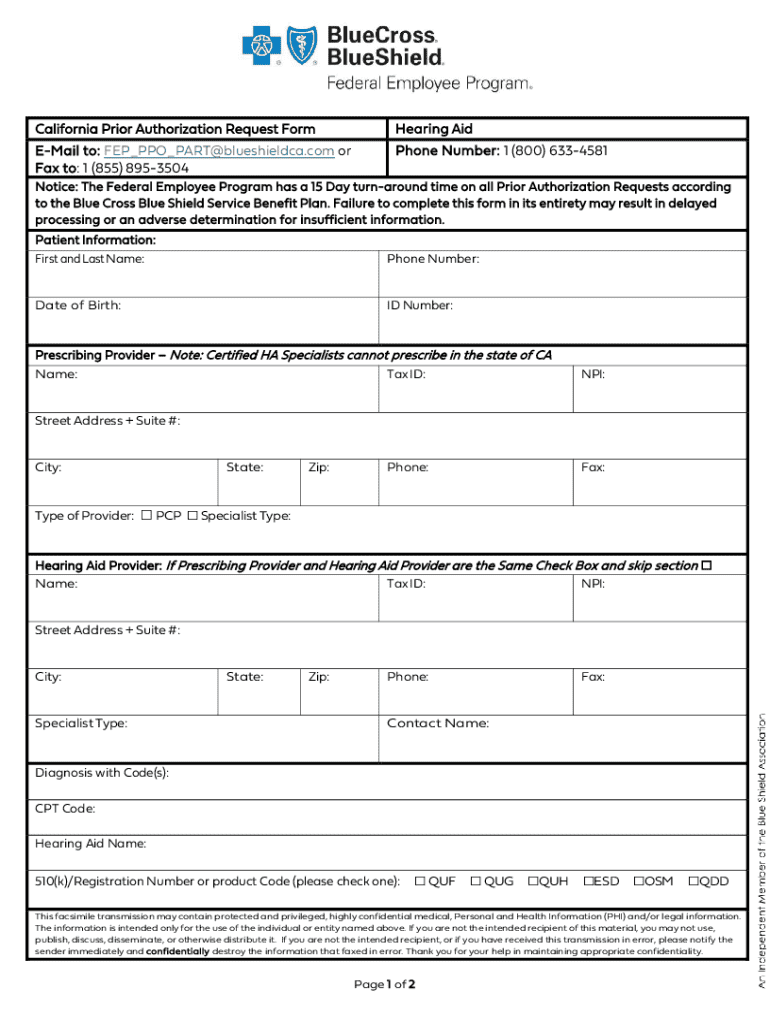
Get the free California Prior Authorization Request Form Hearing Aid E- ...
Get, Create, Make and Sign california prior authorization request
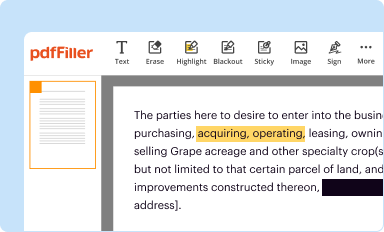
Editing california prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out california prior authorization request
How to fill out california prior authorization request
Who needs california prior authorization request?
California Prior Authorization Request Form: A Comprehensive Guide
Understanding California prior authorization
Prior authorization is a critical process used in California's healthcare system to ensure that specific medical procedures, treatments, or medications are medically necessary before they are covered by health insurance plans. This mechanism plays a significant role in controlling healthcare costs while fostering patient safety by preventing unnecessary procedures.
California has established regulations that dictate how prior authorization must be handled, driven by a joint effort from state health agencies and healthcare providers. These guidelines are primarily designed to streamline the authorization process while protecting patients’ rights and ensuring access to needed care.
Who needs to submit a prior authorization request?
The requirement to submit a prior authorization request typically falls on healthcare providers within the California health system. This includes physicians, hospitals, and outpatient clinics who are seeking approval for their patients’ treatments. However, patients can also be involved, especially when they are navigating their own healthcare access.
This collaborative effort is geared towards ensuring that all parties are compliant with health insurance policies while promoting the best care outcomes for patients.
Key components of the California prior authorization request form
Filling out the California prior authorization request form requires a comprehensive understanding of essential components to prevent delays in treatment. Key elements that must be included are:
While these components are required, providing additional optional information such as previous treatment outcomes or alternative treatment options can enhance the chances of obtaining approval.
Step-by-step guide to filling out the California prior authorization request form
Filling out the California prior authorization request form can seem daunting, but following a systematic approach can simplify the process. Here’s a breakdown of each section of the form:
To ensure accuracy and efficiency, double-check every section for correctness. Consider using tools available on pdfFiller to aid in the completion of your form.
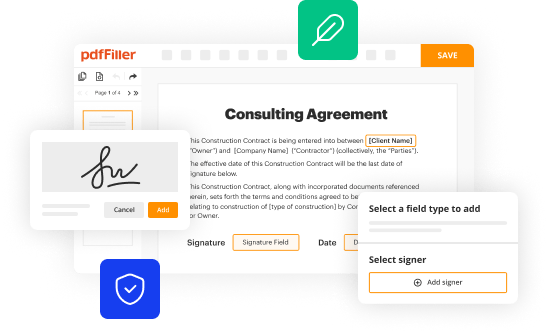
Editing and managing your prior authorization request
Once submitted, the ability to edit prior authorization requests is crucial when seeking to enhance or correct previously submitted information. pdfFiller provides a seamless way to edit and manage your forms. Whether you need to make minor changes or update significant information, follow these steps:
Always keep track of changes and utilize version history features to monitor previous documents. This is vital in maintaining compliance and ensuring effective communication among team members involved in the authorization process.
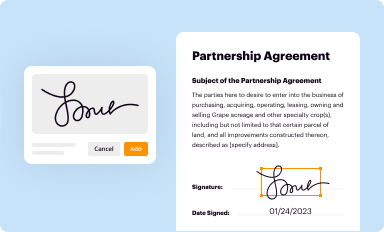
eSigning the California prior authorization request
The eSignature has become an essential component of legal documentation processes across various industries, including healthcare. For the California prior authorization request form, eSigning significantly improves the speed and efficiency of approvals. Steps to eSign your document using pdfFiller include:
Ensuring compliance and security following the signing process is crucial. pdfFiller provides mechanisms to safeguard your documents, ensuring they cannot be altered once signed without proper authorization.
Collaborating with your team
Effective collaboration is vital for any healthcare team managing patient care tasks, including prior authorization requests. pdfFiller enhances team collaboration through several built-in features. Here’s how you can leverage these tools:
These collaborative features are designed to ensure transparency and efficiency, which are essential in managing prior authorization requests.
Tracking the status of your submission
Monitoring the status of your prior authorization submissions is essential to ensure a prompt response from insurance providers. Utilizing pdfFiller, you can easily track your submissions and responses. Steps include:
Establishing a clear communication line with the insurance provider and advocating for timely responses can make a significant difference in managing patient care effectively.
Frequently asked questions (FAQ)
Many individuals may have questions about the California prior authorization request form. Common inquiries revolve around submission processes, eligibility criteria, and what to do if a request is denied. Here are some of the most commonly asked questions:
Understanding the nuances of the prior authorization process can help mitigate confusion and improve advocacy for patient care.
Additional insights and resources
Changes to policies impacting prior authorization in California occur frequently. Keeping up to date is crucial for healthcare providers and teams currently managing patient care. There are various resources available that can help you navigate these changes:
Additionally, pdfFiller offers a variety of accessibility tools for users, making it easier to manage documentation efficiently and effectively.
Final thoughts on utilizing pdfFiller for prior authorization requests
A cloud-based document management platform like pdfFiller significantly streamlines the process of filling out, editing, and managing your California prior authorization request form. Its interactive tools allow healthcare professionals to address documentation needs directly and securely.
Embrace the advantages of using pdfFiller's customized options and features, and explore how the platform can facilitate a seamless workflow. By adopting this technology, teams can enhance their collaborative efforts and advocacy for quick approvals, ultimately leading to improved patient care outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my california prior authorization request in Gmail?
How can I get california prior authorization request?
Can I edit california prior authorization request on an Android device?
What is california prior authorization request?
Who is required to file california prior authorization request?
How to fill out california prior authorization request?
What is the purpose of california prior authorization request?
What information must be reported on california prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.