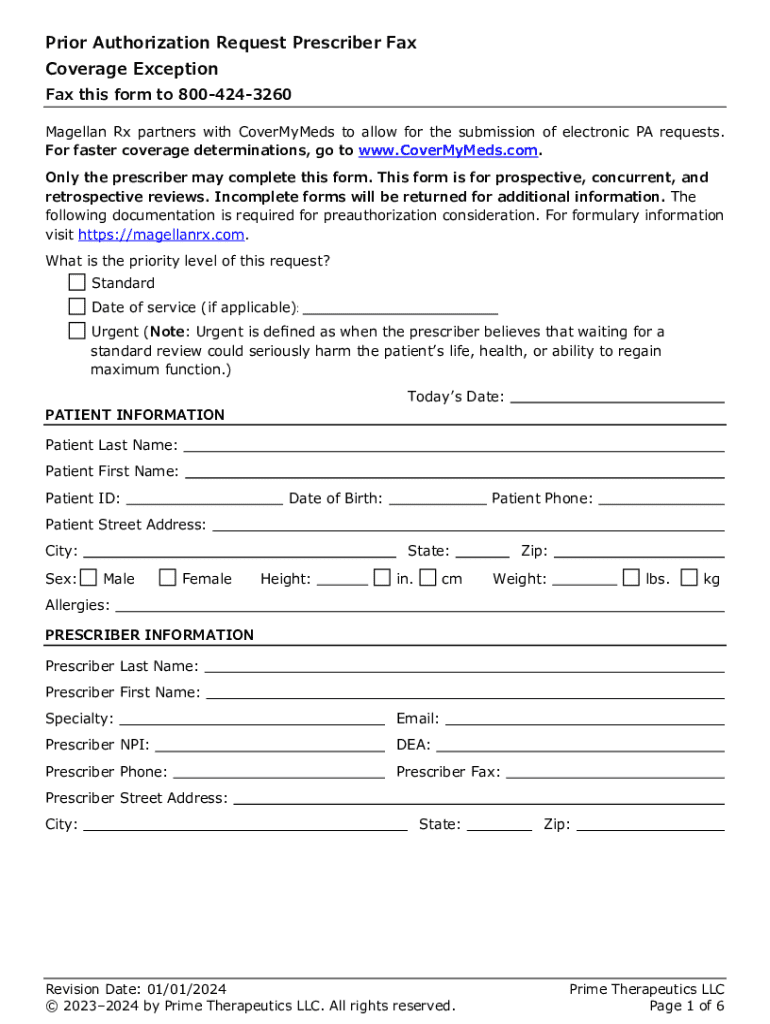
Get the free Coverage Exception Prior Authorization Request Prescriber Fax Form. Coverage Excepti...
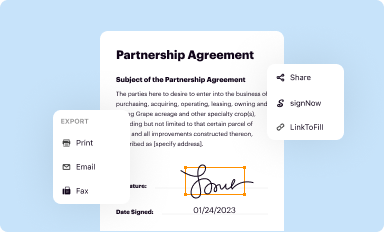
Get, Create, Make and Sign coverage exception prior authorization
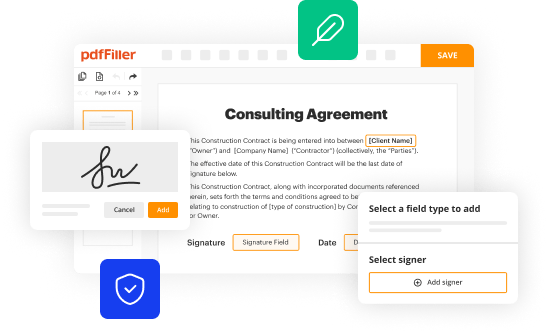
Editing coverage exception prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage exception prior authorization
How to fill out coverage exception prior authorization
Who needs coverage exception prior authorization?
Complete guide to coverage exception prior authorization form
Understanding coverage exception prior authorization
A coverage exception is a critical request made to health insurance providers to access necessary medical treatments or medications that are otherwise not covered under a patient’s current insurance policy. The process of prior authorization is crucial in healthcare as it ensures that both the provider's and policyholder's needs align with the coverage rules established by insurance companies.
Understanding when a coverage exception is necessary can empower patients and healthcare providers alike. Coverage exceptions are typically required for high-cost medications or treatments that are not on the approved list ('formulary') of the insurance plan. This form of prior authorization can help justify the need for specific services or drugs based on individual medical histories.
Overview of the coverage exception prior authorization process
The process of submitting a coverage exception prior authorization request may seem daunting at first, but breaking it down into manageable steps can streamline your experience. Each insurance provider may have its own guidelines; however, the following steps often apply.
Filling out the coverage exception prior authorization form
Completing the coverage exception prior authorization form requires detailed attention to ensure a successful request. Each section is designed to capture pertinent information about both the patient and the required treatment.
Tips for accurate completion include: double-checking patient and provider identifiers, ensuring all clinical justifications are accurately represented, and attaching supporting documentation to reinforce the rationale for the request.
Editing and managing your coverage exception form online
With platforms like pdfFiller, managing your coverage exception prior authorization form becomes far more manageable. Leveraging online tools is beneficial for several reasons.
Utilizing these capabilities not only enhances the accuracy of your submission but also significantly reduces turnaround times.
Tracking the status of your coverage exception request
After submitting your request, staying informed about its status is essential. Most insurance providers allow for online checks or via a dedicated phone line.
Responding to a denial can be as crucial as the initial request; understand the insurance company's appeals process and gather any further information required.
Additional resources for patients and providers
Navigating the complexities of coverage exceptions can be overwhelming. Therefore, having access to various forms of support can make the process smoother.
Best practices for submitting a successful coverage exception request
Submitting a successful coverage exception request often hinges on the thoroughness and clarity of documentation. Building a strong case for approval involves several strategic actions.
These practices can dramatically influence the success of your request and ultimately ensure you receive the necessary treatments without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in coverage exception prior authorization?
Can I create an eSignature for the coverage exception prior authorization in Gmail?
How do I edit coverage exception prior authorization on an iOS device?
What is coverage exception prior authorization?
Who is required to file coverage exception prior authorization?
How to fill out coverage exception prior authorization?
What is the purpose of coverage exception prior authorization?
What information must be reported on coverage exception prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.