Get the free Coordination of Benefits & Recovery Overview
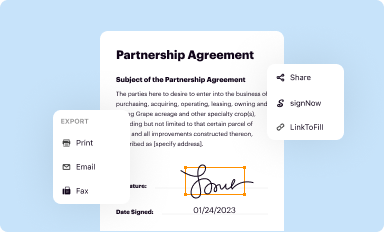
Get, Create, Make and Sign coordination of benefits amp
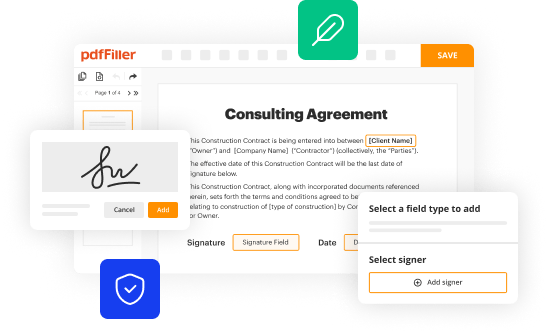
Editing coordination of benefits amp online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coordination of benefits amp
How to fill out coordination of benefits amp
Who needs coordination of benefits amp?
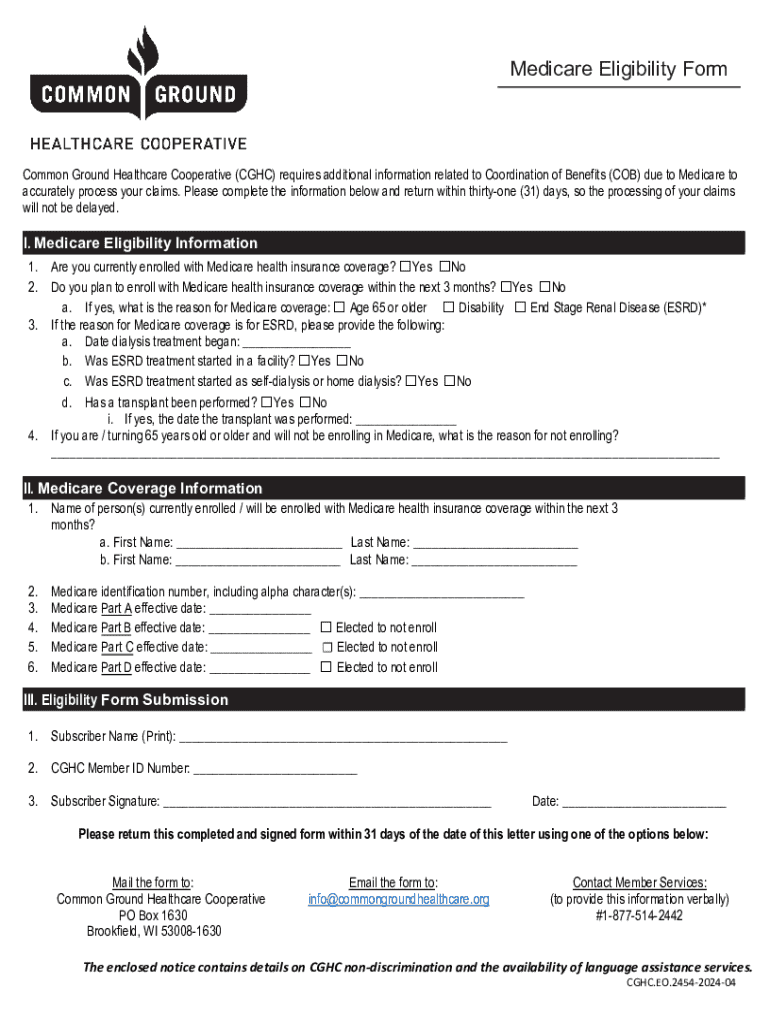
Understanding the Coordination of Benefits AMP Form
. Understanding coordination of benefits (COB)
Coordination of Benefits (COB) refers to the process used by health insurance companies to determine which plan pays first when an individual is covered by multiple health insurance policies. This ensures that there is no duplication of benefits and that healthcare costs are shared appropriately between the insurers. Understanding COB is crucial for policyholders as it impacts claim processing and out-of-pocket expenses.
The importance of COB lies in efficiently managing claims across multiple insurance policies, ultimately protecting the insured from excessive costs. It's vital for individuals with dual coverage to understand the distinctions between primary and secondary insurance roles, as these influence the total amount covered for medical services.
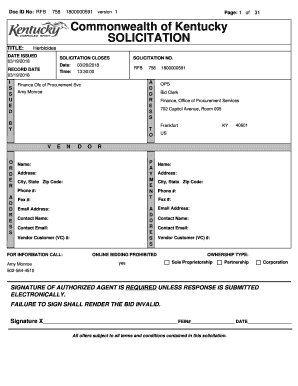
. Overview of the coordination of benefits AMP form
The Coordination of Benefits AMP Form is a specialized document used to facilitate the COB process. Its primary purpose is to collect necessary information from policyholders for efficient claims processing and to clarify the roles of multiple insurance providers.
Key features of the AMP form include sections for personal details, information about additional health insurance, and claim history. This form streamlines communication between insurers and ensures all relevant parties have the same information to evaluate claims properly.
To be eligible to submit an AMP form, the insured must have multiple health insurance policies or be covered by a spouse's or a parent's plan in addition to their own. This form is particularly essential when seeking benefits under both policies.
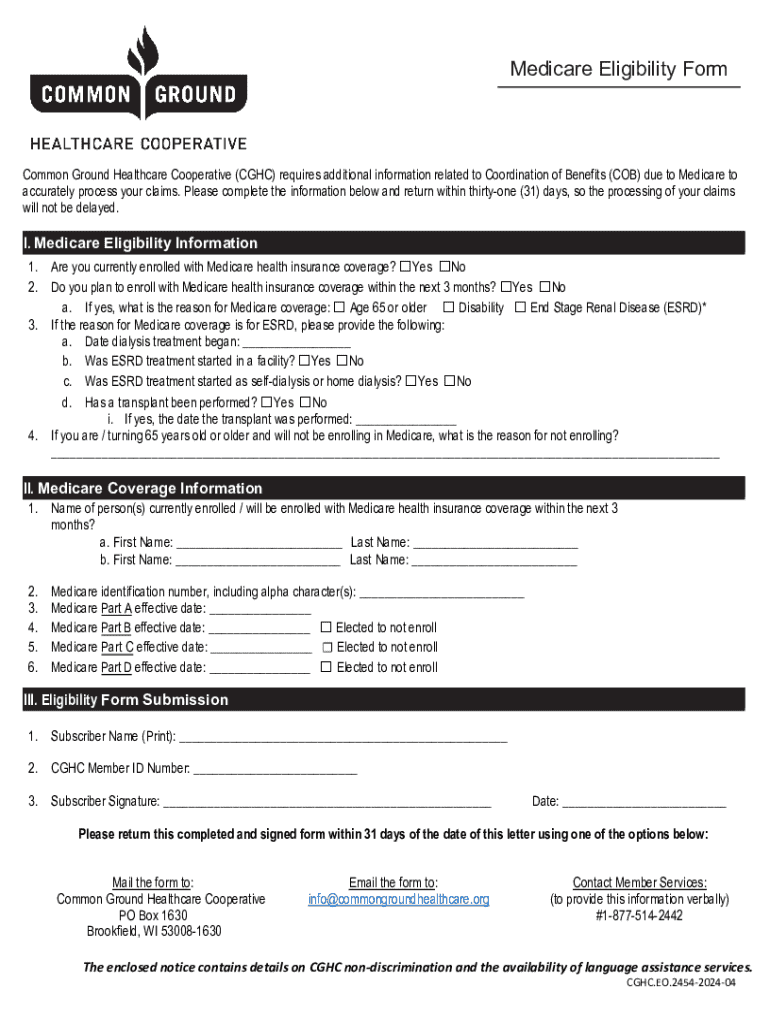
. The process of filling out the coordination of benefits AMP form
Completing the Coordination of Benefits AMP form requires careful attention to detail. Follow these step-by-step instructions to ensure accuracy.
Tips for accurate information submission include double-checking all entries, keeping copies of submitted forms, and understanding the specific requirements of each insurance provider to avoid unnecessary delays.
. Best practices for completing the coordination of benefits AMP form
Many individuals encounter challenges when filling out the Coordination of Benefits AMP form. By adhering to best practices, you can streamline the submission process and reduce errors.
. Managing your coordination of benefits
Understanding how multiple insurance plans work together is essential for maximizing coverage. The primary rules dictate which insurance pays first, while the remaining policy may cover costs that exceed the primary insurance's payment limit.
The pros of having dual coverage include reduced out-of-pocket expenses and greater flexibility in choosing providers. However, challenges may arise such as potential confusion over which plan covers what. It's crucial to evaluate your healthcare needs before committing to dual coverage.
When considering whether to maintain two health insurance plans, it’s important to assess your job benefits, family status, and healthcare requirements to make the best decision suited to your situation.
. Addressing common issues with COB and the AMP form
Common COB issues can include disputes over benefit payments or delays in claim processing. Being proactive about communication with your insurance providers can mitigate these problems.
If you encounter form submission issues, verify that you have completed each section accurately and that all necessary information has been included. Insurance companies can often provide guidance on how to resolve issues.
. Interactive tools and resources for AMP form users
For those seeking assistance with the AMP form, various tools and resources can aid in the process. Templates and checklists can help ensure all necessary sections are filled out, while FAQs provide quick answers to common concerns.
Additionally, having a reliable contact for support can speed up resolution of any issues faced during submission. Seek out customer support representatives from your insurer for personalized guidance.
. Real-life scenarios: Success stories
Numerous individuals have successfully navigated the complexities of COB with the AMP form. For instance, a couple utilizing the form streamlined their claims process, which not only reduced out-of-pocket expenses but also improved their overall experience with coordinating coverage. These success stories encourage others facing similar situations to utilize the form efficiently.
Testimonials highlight how staying organized and informed makes a significant difference in managing multiple insurance plans, emphasizing the importance of proactive engagement and communication.
. Conclusion on leveraging the coordination of benefits AMP form
Staying organized is pivotal when dealing with the Coordination of Benefits AMP form. By understanding the benefits of capturing accurate information, policyholders can leverage their coverage efficiently and avoid common pitfalls. Utilizing tools like pdfFiller can streamline the entire document management process, making it easier to edit, eSign, and collaborate on the AMP form. This single, cloud-based platform will empower you to manage your documents with ease, ensuring that claims are processed smoothly and benefits are maximized.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my coordination of benefits amp directly from Gmail?
How can I get coordination of benefits amp?
Can I create an eSignature for the coordination of benefits amp in Gmail?
What is coordination of benefits?
Who is required to file coordination of benefits?
How to fill out coordination of benefits?
What is the purpose of coordination of benefits?
What information must be reported on coordination of benefits?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.