Get the free Coverage Determination Request ...
Get, Create, Make and Sign coverage determination request
Editing coverage determination request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coverage determination request
How to fill out coverage determination request
Who needs coverage determination request?
Coverage Determination Request Form: A Comprehensive How-to Guide
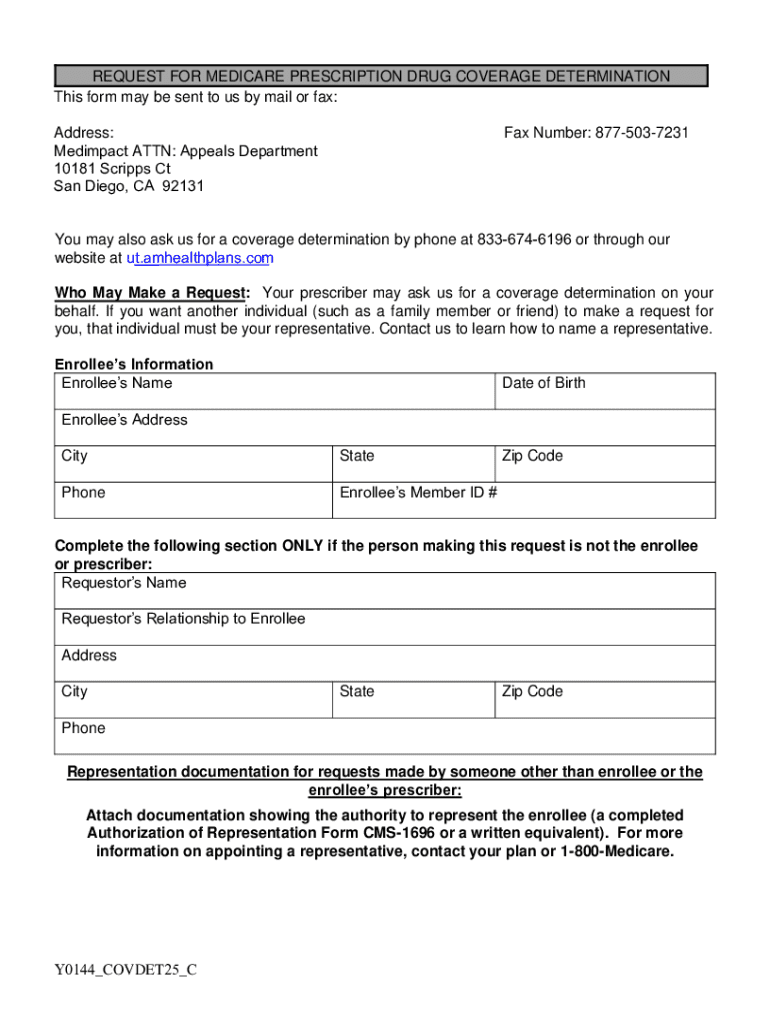
Understanding coverage determination requests
A coverage determination request is a formal appeal made to a health insurance company when a patient, healthcare provider, or caregiver believes that a specific medical treatment, service, or prescription should be covered under the patient's insurance plan. This process plays a vital role in the healthcare system by ensuring that patients receive the appropriate level of care and that insurers are held accountable for their coverage commitments.
The importance of coverage determination within healthcare cannot be overstated. It affects not only the financial aspects of medical care but also the access to necessary treatments. Patients facing severe illnesses often depend on these determinations to secure medications that may be life-saving, underlining how crucial this process is for helping individuals navigate the often-confusing landscape of health insurance.
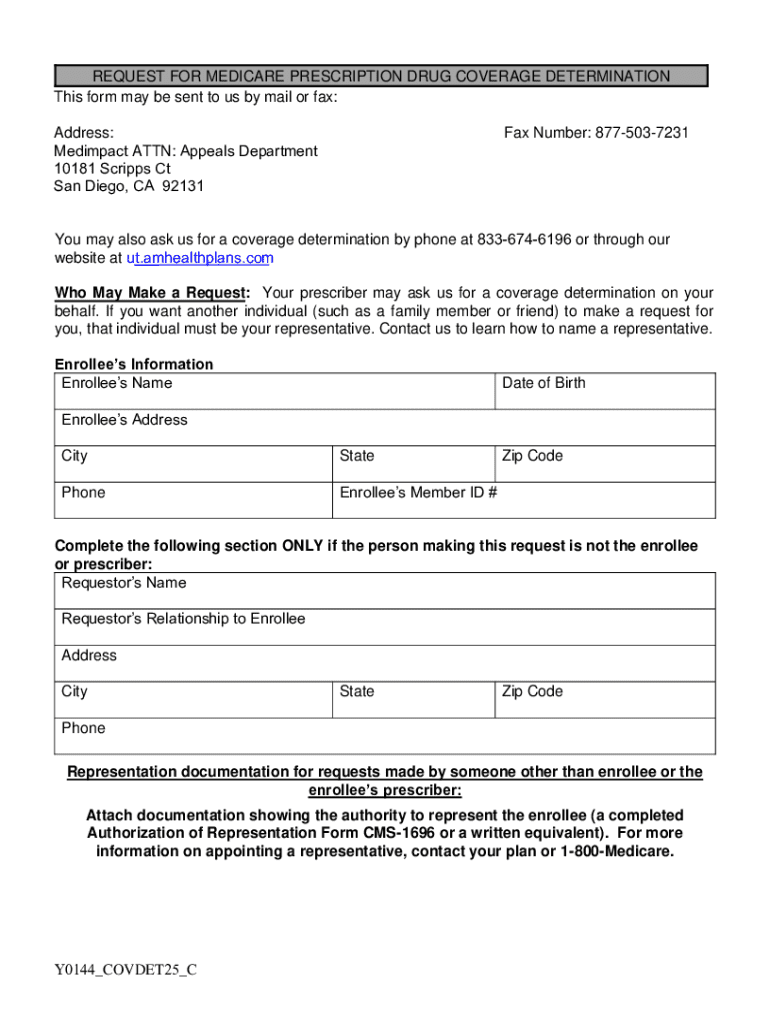
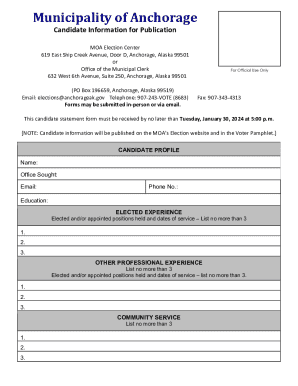
Key components of the coverage determination request form
The coverage determination request form typically consists of several key sections that must be completed accurately to facilitate a swift processing of the request. Understanding each section is crucial for effective submission.
Filling out the coverage determination request form
Completing the coverage determination request form can be straightforward if each section is filled out methodically. Here's a step-by-step approach to ensure your form is filled out correctly.
Common errors can lead to delays or denials. Always double-check for typos or missing information before submitting the form to avoid common pitfalls.
Supporting information for exception requests
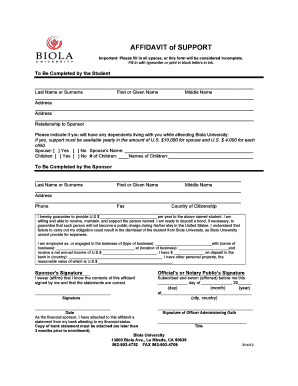
When processing an exception request, additional supporting documentation may be necessary to provide justification for the requested treatment. This information strengthens the case for coverage.
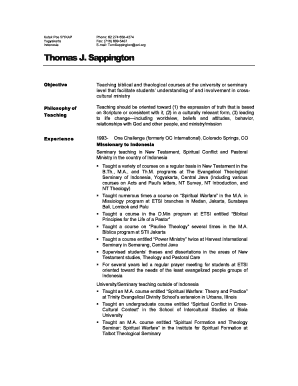
Role of the prescriber
Involving your prescriber is a crucial aspect of the coverage determination process. The prescriber plays an essential role in advocating for necessary treatments and helping to navigate the intricacies of insurance coverage.
When working with your prescriber, it is important to provide them with necessary information, including their contact details and specific details about the required documentation. Coordination is key, as they may need to supply additional documentation or notes to support the request effectively.
Detailed insights on specific coverage types
Different health plans, such as Medicare Advantage Plans and Prescription Drug Plans (PDP), have various coverage determinations that can significantly impact the outcome of your request.
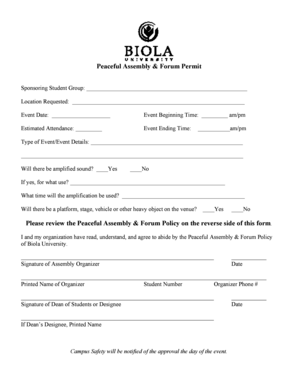
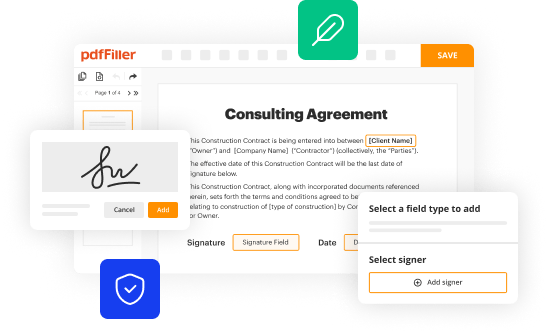
Tools for effective document management
Utilizing tools like pdfFiller can streamline the process of creating and managing your coverage determination request form. With this platform, users can access various features which enhance their experience.
Using pdfFiller’s workflow integration can further enhance document management, allowing for improved tracking of submitted requests and easier access to necessary documentation.
Troubleshooting common issues
It is not uncommon for a coverage determination request to be denied. Familiarize yourself with the next steps in case your request is not approved.
Frequently asked questions
The coverage determination process often raises several questions regarding who may initiate a request and how long the processing may take.
Next steps to take after submission
Once you submit your coverage determination request form, it is essential to understand what follows. Knowing these steps can help manage expectations regarding the outcome.
Importance of understanding your benefits
Being aware of your benefits concerning coverage determination can facilitate a smoother experience. Understanding what services are typically covered ensures that you’re prepared for potential denials and can respond appropriately.
Knowledge of care options and pharmacy access is paramount post-approval. Once coverage is confirmed, knowing which local pharmacies and healthcare providers comply with your plan can reduce further complications.
Continuous support and further learning
Leverage ongoing resource access for document management with platforms like pdfFiller. Continuous learning about health insurance processes and documentation can further empower users and ensure smoother experiences in the future.
Utilizing pdfFiller tools for future requests and forms can simplify the documentation process and enhance your ability to manage future coverage determination requests efficiently.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete coverage determination request online?
How do I edit coverage determination request in Chrome?
Can I edit coverage determination request on an iOS device?
What is coverage determination request?
Who is required to file coverage determination request?
How to fill out coverage determination request?
What is the purpose of coverage determination request?
What information must be reported on coverage determination request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.