Get the free Cystic Fibrosis Drugs Prior Authorization of Benefits Form
Get, Create, Make and Sign cystic fibrosis drugs prior
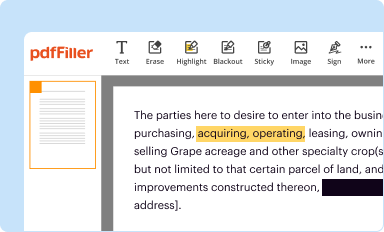
How to edit cystic fibrosis drugs prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cystic fibrosis drugs prior
How to fill out cystic fibrosis drugs prior
Who needs cystic fibrosis drugs prior?
Cystic fibrosis drugs prior form: A comprehensive guide to the prior authorization process
Breadcrumb navigation
Navigating healthcare forms can be challenging. This document provides an easy path to understand the Cystic Fibrosis Drugs Prior Authorization Form and connect to related documents crucial for managing cystic fibrosis treatment.
Understanding cystic fibrosis
Cystic fibrosis (CF) is a genetic disorder that primarily affects the lungs, leading to the accumulation of thick mucus that can cause chronic infections and respiratory issues. The disease can also impact the pancreas, leading to problems with digestion and nutrient absorption. Management of cystic fibrosis requires consistent medical treatment, making medication management critical for improving health outcomes.
Due to the complexity of CF, patients often need a range of medications to manage symptoms and chronic infections. Common drugs prescribed for CF include bronchodilators, mucolytics, antibiotics, and CFTR modulators. These medications are vital for maintaining lung function, preventing infections, and ultimately enhancing quality of life for those living with the disease.
Purpose of the cystic fibrosis drugs prior authorization form
The Cystic Fibrosis Drugs Prior Authorization Form is a pivotal document that assures insurance providers kickstart the requisite approval processes for specific medications. Prior authorization is crucial as it helps control medication costs while ensuring patients receive necessary treatments. Often, rigorous documentation is required to support the need for expensive drugs, especially those that might not fall under standard treatment protocols.
Facilitating access to medications through prior authorization can greatly affect treatment regimes. Successful approval means patients can obtain prescribed medications without facing delays or financial burdens, while denial may necessitate an appeal or alternative treatment plans. Understanding the implications of this process is key for patients, caregivers, and healthcare providers.
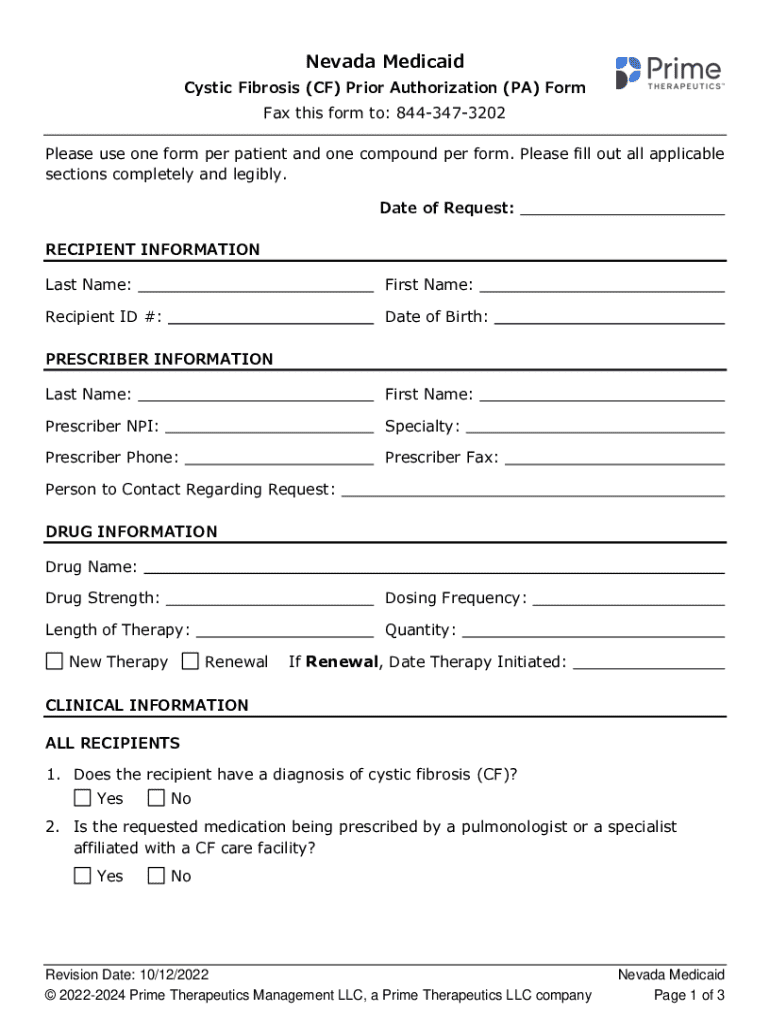
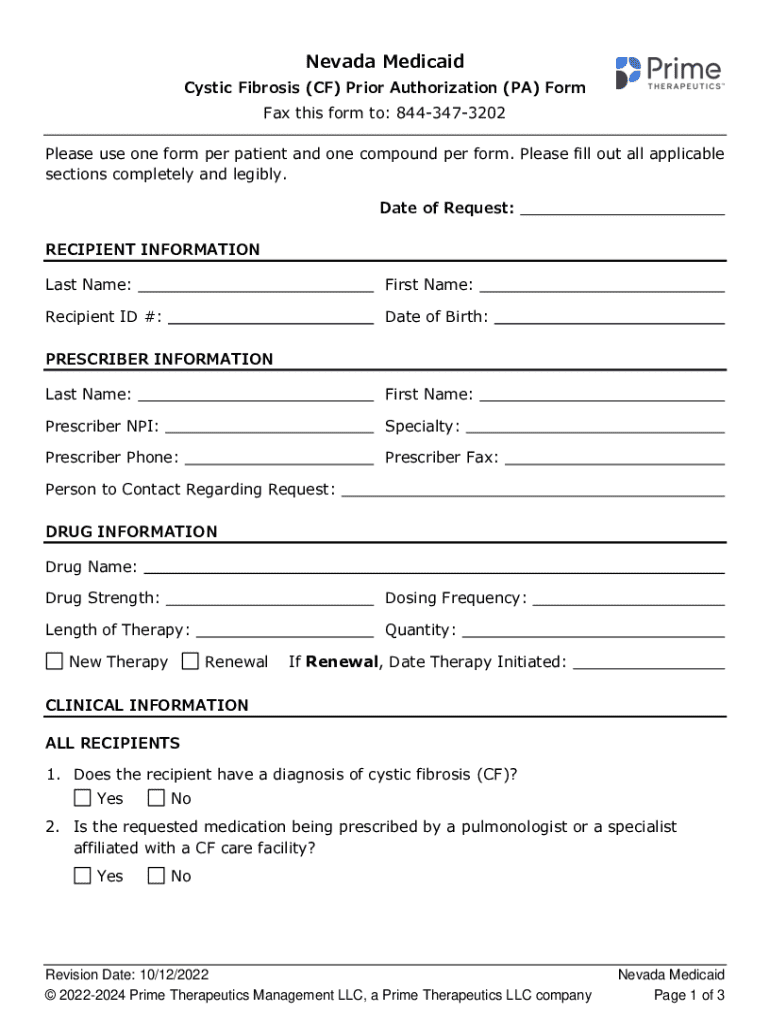
Key elements of the prior authorization form
To effectively complete the Cystic Fibrosis Drugs Prior Authorization Form, certain essential elements must be included. The accuracy of this information is vital for facilitating a smooth approval process.
Step-by-step instructions for filling out the prior authorization form
Completing the Cystic Fibrosis Drugs Prior Authorization Form can seem daunting, but following a structured approach can simplify the process. Here’s how to do it.
Submission process
Once the prior authorization form is complete, understanding the submission process is crucial. Health care providers can submit the form either electronically or via physical copies, depending on the insurance provider’s requirements.
After submission, it's important to be aware of what to expect. Typical processing times for prior authorization approval range from a few hours to several days, depending on the insurer’s protocols and the needs of the request.
Troubleshooting common issues
Delays or denials in prior authorization can occur for various reasons. Understanding these can ease the process of addressing them. For instance, missing information can lead to prolonged waits for approval since insurers may require additional documentation before they can finalize the decision.
Frequently asked questions (FAQs)
As forms and processes can be confusing, many patients and caregivers have common queries that arise during the prior authorization process.
User-friendly tools for document management
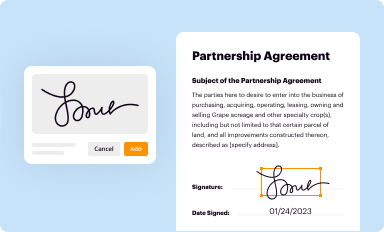
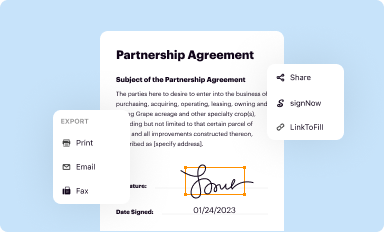
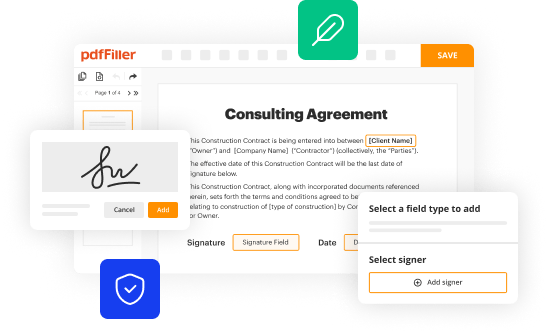
For those managing the Cystic Fibrosis Drugs Prior Authorization Form, utilizing efficient tools can streamline the process. pdfFiller offers an intuitive platform where users can seamlessly edit PDFs, eSign, and manage documents all in one place.
The platform enhances collaborative options for healthcare teams who need to share forms for joint approvals or reviews. These features minimize confusion and improve communication between patients, healthcare providers, and insurance companies.
Best practices for managing medication forms
To ensure ongoing compliance and simplicity in medication management, implementing best practices for handling forms is critical. Regularly update your knowledge on drug changes and new approvals to keep pace with developments in treatment options for cystic fibrosis.
Keep meticulous records of submissions and outcomes, including dates and responses from insurance providers. Engaging actively with healthcare teams will foster a collaborative approach to achieving the best results for cystic fibrosis treatment and ensure that patients receive the necessary medications in a timely manner.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for the cystic fibrosis drugs prior in Chrome?
Can I create an electronic signature for signing my cystic fibrosis drugs prior in Gmail?
How can I edit cystic fibrosis drugs prior on a smartphone?
What is cystic fibrosis drugs prior?
Who is required to file cystic fibrosis drugs prior?
How to fill out cystic fibrosis drugs prior?
What is the purpose of cystic fibrosis drugs prior?
What information must be reported on cystic fibrosis drugs prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.