Get the free kpmas
Get, Create, Make and Sign kpmas form



Editing kpmas form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out kpmas form

How to fill out kpmas md medicaid prior
Who needs kpmas md medicaid prior?
KPMAS Medicaid Prior Form: Your Comprehensive How-To Guide
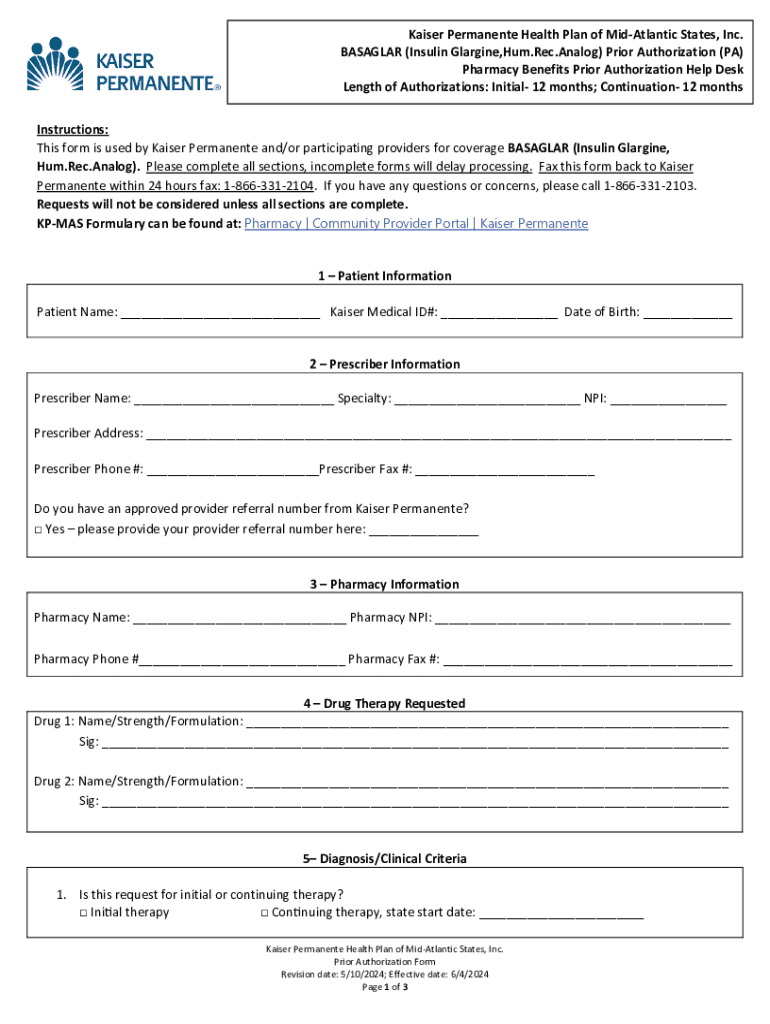
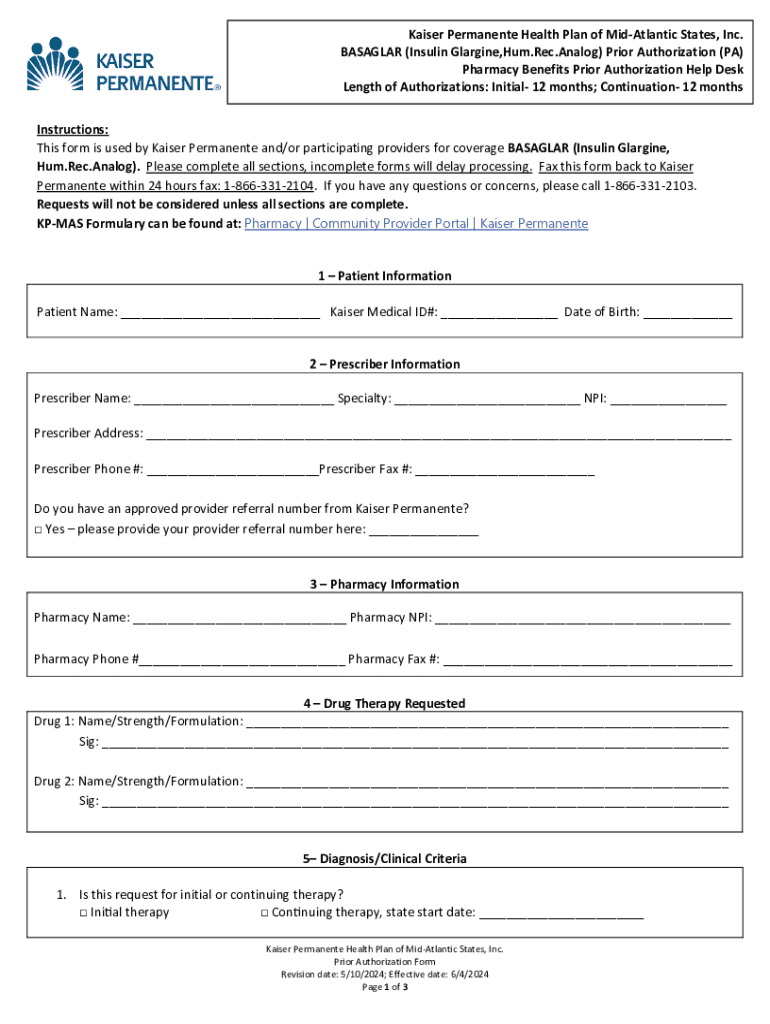
Understanding the KPMAS Medicaid Prior Form
The KPMAS MD Medicaid Prior Form is a crucial document for patients seeking necessary medical services through Medicaid in Maryland. This form is essential because it serves as a request for prior authorization from the Medicaid program, guaranteeing that the proposed services are covered under the beneficiary's plan.
Obtaining prior authorization is a significant step for Medicaid beneficiaries, ensuring that the medical treatments or services they seek are approved before being rendered. This can help prevent unexpected costs and delays in care, which is especially important for those who rely on Medicaid for essential services.
Who Needs the Form?
Eligibility for Medicaid in Maryland includes individuals and families with low income, pregnant women, children, elderly individuals, and people with disabilities. If you fall into any of these categories, you may be required to complete the KPMAS MD Medicaid Prior Form under specific circumstances.
Typical situations necessitating the form include specialized services not directly covered under your Medicaid plan, such as certain surgeries, durable medical equipment, or extended therapy sessions. By completing this form, providers can justify the need for these services based on medical necessity.
Key Components of the KPMAS Medicaid Prior Form
The KPMAS MD Medicaid Prior Form contains several critical sections designed to gather comprehensive information necessary for the review process. Understanding each component can significantly aid in completing the form accurately, thus improving the likelihood of approval.
Each section—Patient Information, Provider Information, and Medical Necessity Justifications—requires careful attention. For example, accurate patient details are crucial as the information directly links to the beneficiary’s Medicaid plan and helps in assessing eligibility for the required services.
Step-by-step instructions for filling out the form
Before starting to fill out the KPMAS MD Medicaid Prior Form, it’s beneficial to gather all necessary documentation related to both the patient’s medical history and the specific service being requested. This preparation lays the foundation for a complete and well-supported application.
Tips for ensuring a successful submission
Completing the KPMAS MD Medicaid Prior Form meticulously can significantly reduce the chances of delays or denials in the review process. One common mistake to avoid is leaving any sections incomplete. This could cause the reviewing team to reject or request additional information, prolonging care.
Legibility and clarity are vital for a successful submission. Using a clear format and avoiding handwriting can help ensure that the form is read accurately. Submissions that are clearly articulated are often processed faster, leading to quicker approvals.
Understanding the review process
Once the KPMAS MD Medicaid Prior Form is submitted, it enters a review process conducted by Medicaid officials. Typically, you can expect a timeline of about 5 to 10 business days for the review to be completed, depending on the complexity of the case and the volume of requests being processed.
The outcome may vary: approval, denial, or request for additional information. If a denial occurs, the form typically includes an explanation along with instructions on how to appeal the decision. Utilizing the right approach when addressing denials can help facilitate alternative routes to securing coverage.
Tools for managing the KPMAS Medicaid Prior Form
Managing documents can often become overwhelming, especially in healthcare. Tools like pdfFiller make it easier to edit, eSign, and securely store the KPMAS MD Medicaid Prior Form. This cloud-based platform allows users to fill out forms anywhere, increasing accessibility and convenience.
Collaboration is also streamlined within pdfFiller. You can easily share the form with medical or administrative staff for additional input or edits, ensuring that all necessary details are accurately captured before final submission.
Frequently asked questions (FAQs)
You may have questions regarding the KPMAS MD Medicaid Prior Form. One common query pertains to processing time—approximately 5 to 10 business days is standard. Additionally, many wonder if the form can be submitted online. Various providers now offer electronic submission options, streamlining the entire process.
Another frequent question is about resubmission if more information is requested after submission. In such cases, it is crucial to respond promptly with the requested details to avoid further delays in approval.
Final steps and follow-up
Staying informed after submitting the KPMAS MD Medicaid Prior Form is vital. Keeping track of your submission status can prevent unnecessary anxiety and provide clarity on timelines. It is advisable to establish contact with the Medicaid office for any updates related to your application, which can also help expedite any pending requests.
Be proactive in your follow-ups and document any interactions you have. This can serve as evidence in case of disputes or further complications. Establishing a clear line of communication can significantly simplify the overall process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get kpmas form?
How do I edit kpmas form on an Android device?
How do I fill out kpmas form on an Android device?
What is kpmas md medicaid prior?
Who is required to file kpmas md medicaid prior?
How to fill out kpmas md medicaid prior?
What is the purpose of kpmas md medicaid prior?
What information must be reported on kpmas md medicaid prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.