Get the free Provider Network Request Form
Get, Create, Make and Sign provider network request form
Editing provider network request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out provider network request form
How to fill out provider network request form
Who needs provider network request form?
Provider Network Request Form: A Comprehensive Guide
Understanding the provider network request form
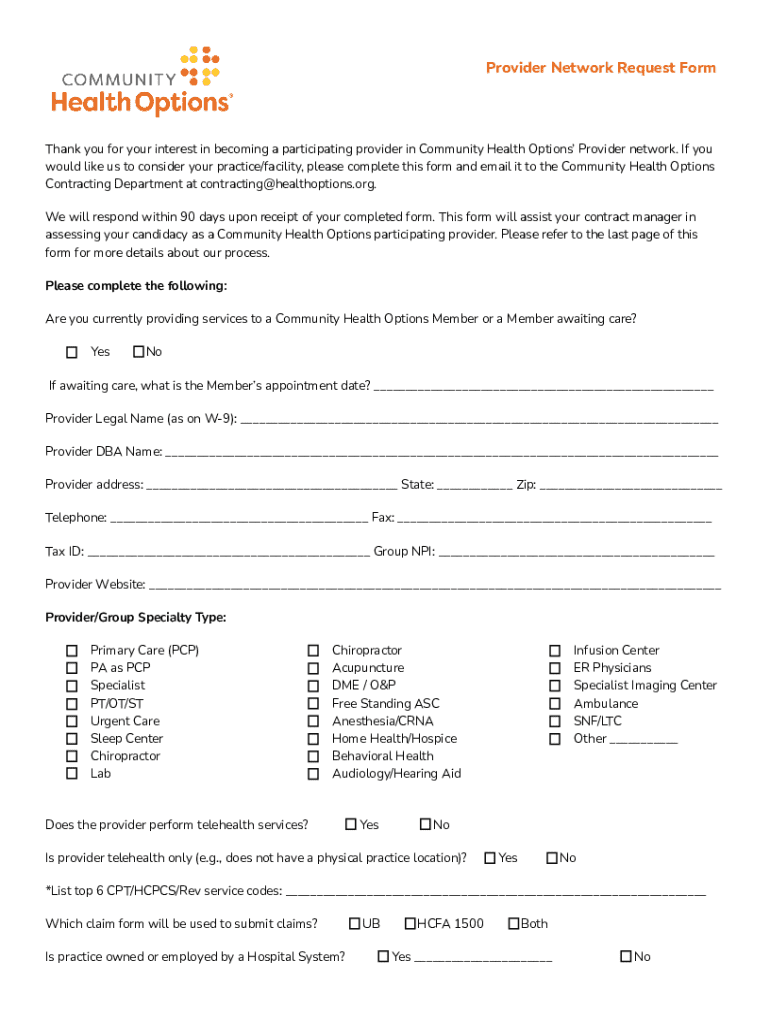
A provider network request form is a crucial document that healthcare providers must complete to join a healthcare network. Its primary purpose is to facilitate the enrollment of individual practitioners or organizations in health insurance plans and managed care organizations. This form collects essential information required for a thorough assessment of the provider's credentials and qualifications, ensuring compliance with network standards.
The key benefits of using the provider network request form include the streamlining of enrollment processes and improved accuracy. By standardizing required information, it reduces the likelihood of incomplete submissions, enhancing compliance with regulatory standards. Additionally, effective communication between healthcare providers and networks can be fostered through detailed requests and evaluations.
Who needs the provider network request form?
The target audience for the provider network request form broadly includes individual healthcare providers, medical groups, practices, and administrative teams within healthcare organizations. Physicians, specialists, nurses, and allied health professionals must become part of a network to practice within certain insurance frameworks, and the request form is their gateway to this opportunity.
Common situations that necessitate the submission of the provider network request form typically involve professionals seeking to expand their practice, change their insurance affiliations, or establish new contracts with managed care organizations. Each scenario requires detailed documentation to ensure compliance and satisfaction within the respective network.
Overview of the provider network request process
Navigating the provider network request process involves several key steps that ensure everything is completed correctly. Starting with initial preparation, providers need to gather all relevant documentation and information before completing the form. This preparation phase sets the foundation for a seamless submission.
Filling out the provider network request form
Filling out the provider network request form requires attention to detail in various sections. The personal information section captures essential details such as the provider's name, contact information, and relevant demographic data. Following this, the license and certification details section is critical to verify qualifications and credentials.
The practice location and setting section provides insight into where healthcare services will be rendered, which is imperative for network planning. Lastly, accurate insurance information ensures that providers align with appropriate coverage plans. Fictional examples or placeholders can create confusion, so attention to accuracy is paramount.
Common mistakes to avoid while filling out the form include submitting incomplete information, incorrectly formatting dates and numbers, and failing to attach necessary supporting documentation. Each of these errors can lead to delays in the application process.
Editing and updating your provider network request form
Accessing the provider network request form for edits is straightforward. Users can log into their accounts on the platform offering the form and locate the document in their files. It’s essential to keep this form updated with the most current information about licenses, practice settings, and insurance policies.
When making updates, ensure that all information is accurate and relevant. Include recent credentials, reflecting any new certifications or changes in practice locations. This diligence enhances the integrity of your application and maintains compliance with network requirements.
Submitting the provider network request form
Submission procedures for the provider network request form can vary significantly, often allowing for both online submission and postal mail. Online forms typically streamline the process, making it easy for providers to attach necessary documentation electronically. Conversely, postal submissions may necessitate additional steps to ensure that all required attachments are included.
It's crucial to confirm receipt of your submission. Providers can often check the status through online portals or by contacting customer service. If confirmation doesn’t arrive within a reasonable timeframe, it’s advisable to follow up to ensure that your application is being processed adequately.
After submission: what to expect
After submitting the provider network request form, providers can anticipate a review process that assesses various criteria spanning their credentials, experience, and compliance with network standards. The timeline for processing requests can widely vary based on the specific network’s protocols. Typically, providers may expect a response within several weeks; however, this may fluctuate.
Potential outcomes include acceptance into the network, requests for additional information to clarify details, or, unfortunately, denial of the request. In the case of a denial, understanding the reasons behind it allows providers to address specific areas of concern before reapplying.
Interactive tools for the provider network request process
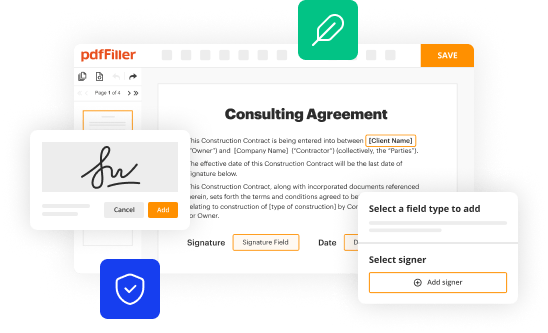
Utilizing pdfFiller features can greatly enhance the experience of completing the provider network request form. The editing capabilities allow healthcare providers to manage documents easily, adjusting information as necessary with user-friendly tools. This adaptability is particularly useful for submitting multiple forms as circumstances change.
The eSign feature facilitates quick approvals and streamlines the document review process. Additionally, collaboration tools enable teams to work together efficiently when managing submissions, making it easier for administrative staff to coordinate and support providers in their applications.
Troubleshooting common issues with the provider network request form
Providers may encounter various challenges while completing the provider network request form, including technical difficulties with online submission tools or issues related to documentation requirements. Understanding these common barriers is the first step toward overcoming them.
In the event of persistent issues, contacting support is vital. Resources like pdfFiller provide customer support that can assist users in addressing their concerns. It's important for providers to keep vital contact information handy to ensure they can quickly resolve any problems.
Best practices for managing your provider network documentation
Keeping records organized is paramount when dealing with provider network documentation. Implementing a systematic approach ensures that critical information is readily available during the application process. Cloud-based solutions can provide the flexibility necessary for healthcare providers to access documentation from anywhere at any time.
Regularly updating information is another best practice. Maintaining accurate records not only assists in immediate applications but also helps in future networking opportunities. Providers who remain proactive in keeping their files current will find it easier to manage the complexities of joining multiple networks or maintaining compliance with evolving healthcare policies.
Success stories: real-world applications of the provider network request form
Real-world applications of the provider network request form illustrate its impact on healthcare practices. Many providers have successfully navigated the enrollment processes, often receiving rapid approvals due to thorough and well-organized submissions. These success stories serve not only as inspiration but also as a guide for best practices in completing applications.
Testimonials from users highlight how efficiently they joined networks, substantially broadening their patient base and enhancing their practice's viability. By leveraging the appropriate tools and resources, providers can optimize their applications to thrive in today’s complex healthcare landscape.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get provider network request form?
How do I complete provider network request form online?
Can I create an eSignature for the provider network request form in Gmail?
What is provider network request form?
Who is required to file provider network request form?
How to fill out provider network request form?
What is the purpose of provider network request form?
What information must be reported on provider network request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.