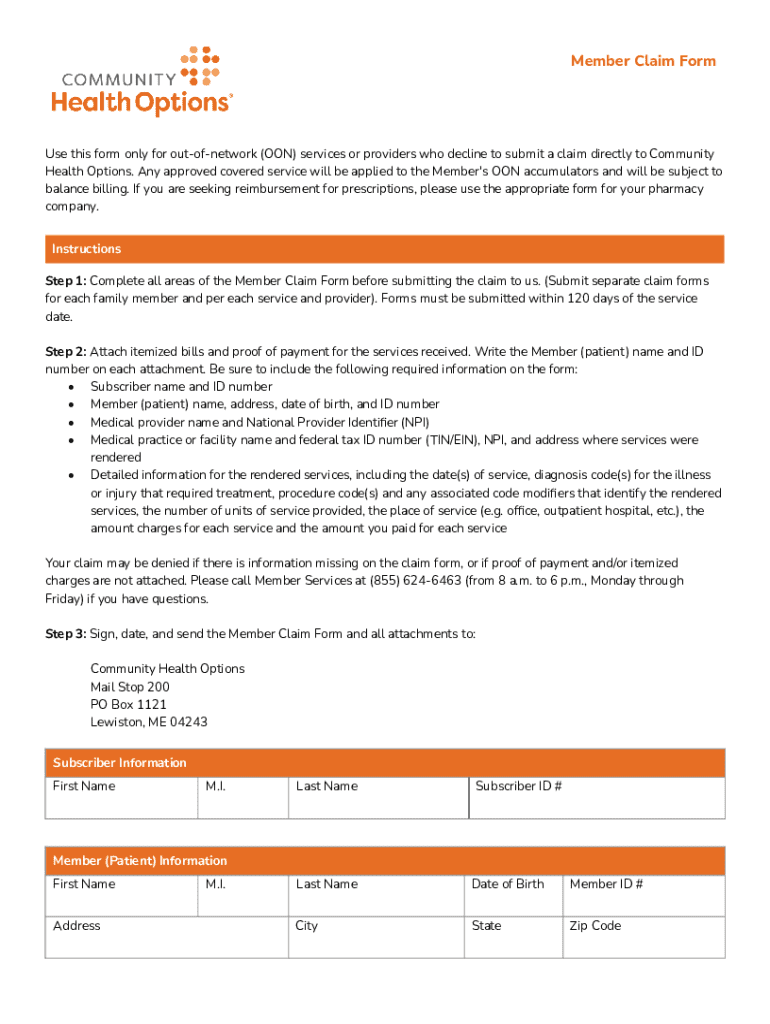
Get the free Member Claim Form
Get, Create, Make and Sign member claim form
How to edit member claim form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out member claim form
How to fill out member claim form
Who needs member claim form?
Your Complete Guide to the Member Claim Form
Understanding the member claim form
A member claim form is a critical document used in the healthcare system to request reimbursement for covered medical services. This form outlines the expenses incurred by a member and serves to facilitate the processing of claims by insurance providers. It enables members to claim back costs associated with healthcare services, ensuring they receive the benefits entitled to them under their insurance policy.
The importance of the member claim form cannot be overstated. Without it, insurance companies have no formal way to process and approve claims, leaving members without much-needed reimbursement. Furthermore, it acts as a record, helping insurance providers track claims submitted and payments made. Essentially, this form is your formal request for financial assistance regarding your healthcare costs.
Who should use the member claim form? Primarily, it is utilized by individuals covered under a health insurance plan when they have out-of-pocket medical expenses. This includes anyone who has paid for their healthcare services upfront and is now seeking reimbursement. Additional users may include healthcare providers submitting claims on behalf of patients.
Types of member claim forms
There are several types of member claim forms, each catering to specific needs in the healthcare sector. Understanding the nuances of each can significantly streamline the reimbursement process.
Additionally, there are specialized forms to address specific healthcare needs. For instance, the Pregnancy Blood Pressure Monitor Request Form allows members to request medical equipment relevant to their condition, while the Contraceptive Exception Form lets individuals exempt certain contraceptive methods from standard co-pay rules.
Step-by-step guide to filling out the member claim form
Filling out the member claim form accurately is vital to ensure a smooth claims process. Here’s a step-by-step breakdown.
Submission process for the member claim form
The submission process for a member claim form is straightforward, but knowing how to submit it effectively can save time and ensure quicker processing.
Tracking your claim status
Once submitted, tracking the status of your claim is essential for timely updates and receipts. Most insurance providers will allow you to access your claims status through their website or via phone.
Common issues during claim processing
Encountering issues during the claim process is common and can be frustrating. Awareness of these issues can help you navigate the process more efficiently.
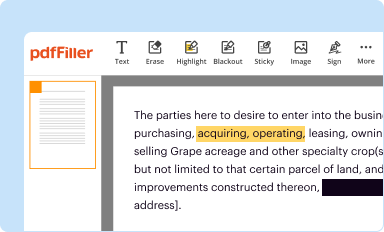
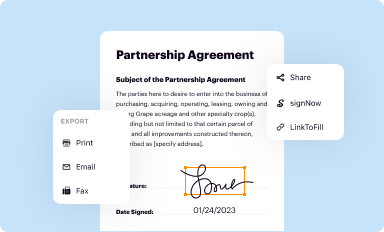
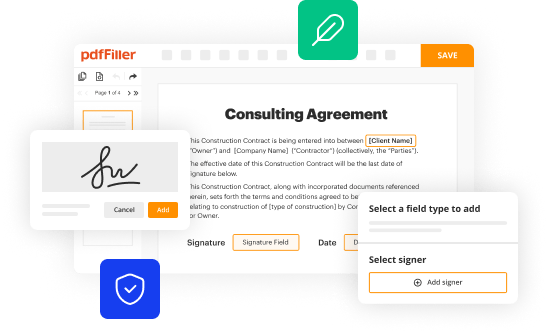
Interactive tools and resources on pdfFiller
Utilizing interactive tools can significantly ease the burden of managing your member claim form. pdfFiller offers a range of features tailored towards simplifying this process.
Additional considerations
Navigating the member claim form landscape requires understanding the finer details that can impact your claims. Different insurance plans may have variations in how claims are processed, including unique documentation requirements and approval timelines.
Getting help and support
If you encounter obstacles while filling out your member claim form, don’t hesitate to seek help. There are several resources available to you.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in member claim form?
How do I make edits in member claim form without leaving Chrome?
How can I edit member claim form on a smartphone?
What is member claim form?
Who is required to file member claim form?
How to fill out member claim form?
What is the purpose of member claim form?
What information must be reported on member claim form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.