Get the free Diet Progression After Esophageal Surgery
Get, Create, Make and Sign diet progression after esophageal
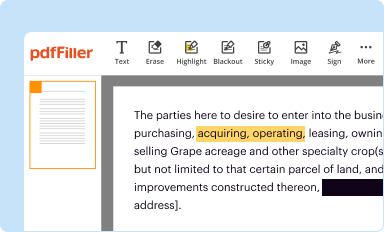
How to edit diet progression after esophageal online
Uncompromising security for your PDF editing and eSignature needs
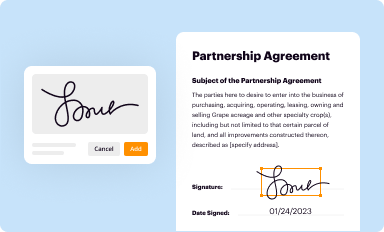
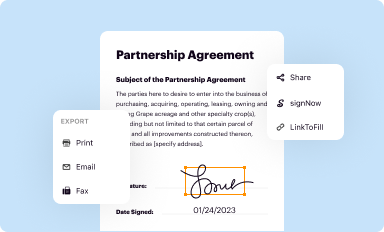
How to fill out diet progression after esophageal
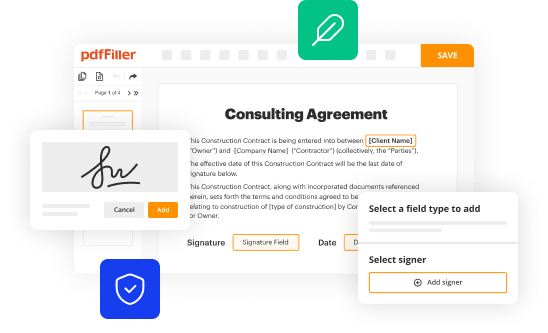
How to fill out diet progression after esophageal
Who needs diet progression after esophageal?
Diet progression after esophageal form: A comprehensive guide
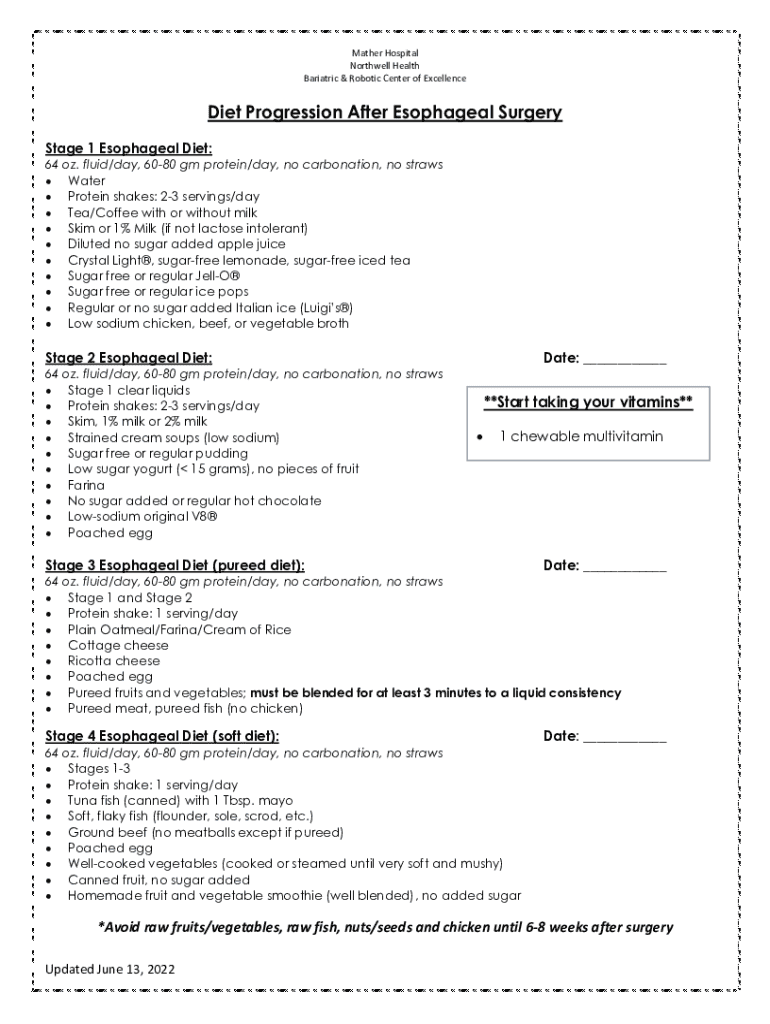
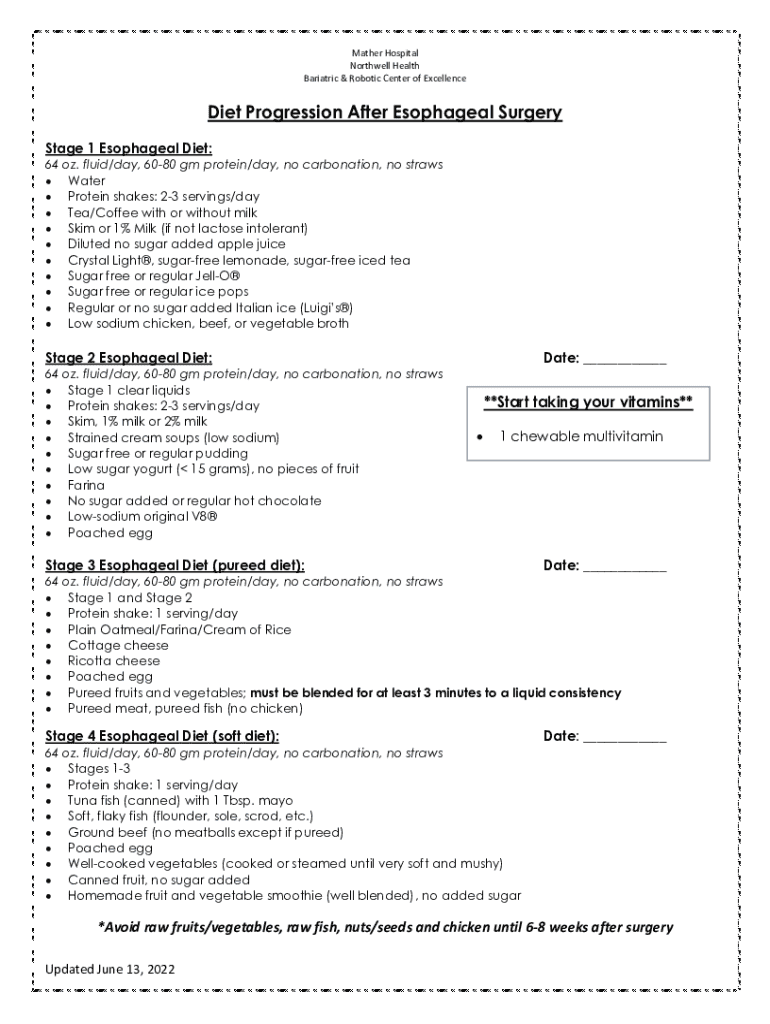
Understanding diet progression post-esophageal surgery
Esophageal surgery, which often includes procedures like esophagectomy or fundoplication, can significantly impact a patient’s diet and nutritional intake. After such surgery, the body's ability to accept and process food changes, necessitating a structured diet progression. Postoperative patients often face challenges such as altered swallowing, changes in appetite, and the need for careful food selection to promote healing.
Nutritional management is critical for recovery and long-term health. Inadequate nutrition can lead to complications like weight loss, malnutrition, and slower recovery times. It's essential to understand how to transition through various dietary phases to ensure the body receives adequate nutrients without causing discomfort or complications.
Phases of diet progression
The diet progression after esophageal surgery is typically broken into several phases, each tailored to accommodate the body's healing process and adjust to new eating patterns.
Immediate postoperative phase (Days 1-2)
During the immediate postoperative phase, the diet primarily consists of liquids as the body begins to recover. Hydration is crucial during this period to prevent dehydration, especially after anesthesia and surgery.
Patients are encouraged to consume clear liquids, such as broth, gelatin, and clear juices. It's important to avoid carbonated and caffeinated beverages, as they can increase bloating and discomfort.
Soft foods introduction (Days 3-7)
As recovery progresses into the third day, patients can begin to incorporate soft foods. This transitional phase allows for nutrient-dense options that are easy to chew and swallow, helping to minimize discomfort.
Suitable soft foods include mashed potatoes, yogurt, and smoothies. Cooking methods such as steaming or pureeing can make foods easier to digest and consume, ensuring a smoother transition from liquids to solids.
Gradual introduction of solid foods (Weeks 2-4)
By weeks two to four, patients can gradually introduce more solid foods into their diet. This stage involves listening to one’s body and recognizing its tolerance levels. Foods like well-cooked vegetables and tender meats can be included as long as they are easy to chew and swallow.
Monitoring signs of intolerance is crucial. Patients should eat slowly and chew each bite thoroughly to facilitate digestion and prevent complications. Attentiveness to body signals during meals, such as discomfort or difficulty swallowing, is essential for making necessary adjustments.
Incorporating a wider variety of foods (Weeks 4-8)
After the initial four weeks, patients can begin to incorporate a wider variety of foods. This stage is pivotal for building a balanced diet that includes various food groups such as grains, fruits, and proteins.
While diversifying your diet, it's important to avoid troublesome foods known to cause discomfort. Spicy, acidic, and hard foods should be minimized during this phase. Nutritional supplements may be beneficial if dietary restrictions significantly limit nutrient intake.
Nutrition guidelines for esophageal surgery recovery
Post-esophageal surgery nutrition is crucial for recovery. Understanding caloric requirements and establishing a balanced macronutrient distribution will help ensure adequate support for healing.
Nutritional needs and considerations
Estimating daily calorie intake should be a personalized approach, as it varies depending on factors like age, weight, and activity level. Patients may need higher caloric intake initially post-surgery due to healing demands.
Balanced nutrition is vital for recovery; plan to include a mix of proteins, carbohydrates, and healthy fats in meals. A typical macronutrient distribution might suggest approximately 20-30% calories from protein, 50-60% from carbohydrates, and 20-30% from fats.
Managing common post-surgery issues
Patients often encounter common issues such as heartburn and reflux, which can be exacerbated by certain foods. Identifying these triggers is vital to avoiding discomfort during the recovery phase.
Additionally, gas and bloating can occur after meals. Keeping a food diary may help pinpoint specific foods that trigger these symptoms and guide dietary adjustments.
Potential complications
Being informed about potential complications is crucial. Dumping syndrome, characterized by rapid gastric emptying, can lead to symptoms such as nausea, weakness, and diarrhea, especially after consuming high-sugar foods.
Dysphagia, or difficulty swallowing, can be another concern for patients. If swallowing problems persist, professional guidance and modifications to the diet may be required.
Creating a sustainable meal plan
Developing a sustainable meal plan is essential for a smooth transition back to regular eating habits. A sample meal plan for the first eight weeks can serve as a practical guide to ensure dietary adherence.
Consider various meal options week by week, gradually increasing the variety while sticking to the recommended food groups.
Tools and resources for navigating post-surgery diet
Utilizing interactive meal planning tools can aid patients in creating customized meal plans. These digital resources allow you to input dietary preferences, restrictions, and nutritional needs, providing tailored meal suggestions.
Keeping a diet journal can also provide insight into food tolerances and preferences, making it easier to adjust meals according to individual needs.
Caregiver support and involvement
Caregivers play a vital role in supporting patients’ dietary needs after esophageal surgery. They can assist with meal preparation and encourage adherence to the dietary plan, ensuring that patients are consuming the right foods for recovery.
Empowering patients to advocate for their nutritional needs contributes to a collaborative recovery journey. Encouraging discussions about food preferences and dietary adjustments fosters a sense of independence and agency in patients.
Summary of key dietary takeaways
Key insights for successful diet progression include understanding the phased approach to returning to a normal diet, recognizing the importance of hydration, and being mindful of food choices. Consultation with healthcare providers remains paramount for personalized dietary recommendations throughout recovery.
Advanced topics in diet and nutrition post-esophageal surgery
Long-term dietary adjustments may be necessary following esophageal surgery. Strategies for lifelong healthy eating can include focusing on nutrient-dense foods and maintaining a balanced intake of macronutrients.
Staying informed about ongoing nutrition strategies in relation to esophageal health is crucial. Joining support groups or nutrition education programs can provide continual guidance as dietary needs evolve.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find diet progression after esophageal?
How do I edit diet progression after esophageal on an Android device?
How do I fill out diet progression after esophageal on an Android device?
What is diet progression after esophageal?
Who is required to file diet progression after esophageal?
How to fill out diet progression after esophageal?
What is the purpose of diet progression after esophageal?
What information must be reported on diet progression after esophageal?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.