Get the free 42 USC 1396a: State plans for medical assistance
Get, Create, Make and Sign 42 usc 1396a state
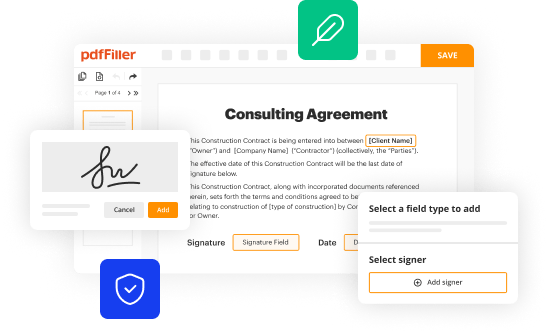
How to edit 42 usc 1396a state online
Uncompromising security for your PDF editing and eSignature needs
How to fill out 42 usc 1396a state
How to fill out 42 usc 1396a state
Who needs 42 usc 1396a state?
42 USC 1396a State Form: A Comprehensive Guide
Overview of 42 USC 1396a
42 USC 1396a plays an essential role in shaping Medicaid policy across the United States. This section of the Social Security Act outlines the requirements state governments must meet in their plans to provide medical assistance to eligible individuals. Understanding these requirements is crucial for states, health providers, and beneficiaries who navigate the complexities of health services funded by Medicaid.
Key terms include "state plan," which is essentially a blueprint that describes how states administer their Medicaid programs, and "medical assistance," which collectively refers to services and benefits provided to eligible individuals.
Understanding state plans for medical assistance
State plans under 42 USC 1396a serve as a formal document indicating the methods and operations states will employ to deliver Medicaid services. The purpose of these plans is straightforward: to ensure states adhere to federal guidelines while addressing the unique healthcare needs of their populations. Each state must submit its plan for approval to the Secretary of Health and Human Services, ensuring compliance with federal Medicaid standards.
The validity of a state plan hinges on several key components. These include the description of the Medicaid program, financial controls, the available services, and the qualifications for beneficiaries. The Secretary’s role in this process is critical, as they review and either approve or disapprove these plans based on adherence to federal requirements, which helps maintain uniformity and quality in Medicaid services across states.
Content requirements of state plans
The contents of a valid state plan as outlined in 42 USC 1396a are detailed in subsections (a) through (z). Each element serves a purpose to ensure comprehensive coverage and stringent oversight.
Eligibility criteria and coverage options
Eligibility requirements for Medicaid programs under 42 USC 1396a are clearly defined in subsections (k) and (l). It specifies the minimum conditions for coverage, which includes who qualifies as aged, blind, or disabled, alongside income thresholds that must be met.
Optional coverage categories found in subsections (hh) and (ii) offer states opportunities to expand Medicaid to families and individuals who may not meet traditional requirements. This flexibility allows for broader access to essential medical services, which is especially beneficial in states that wish to implement additional safety nets for vulnerable populations.
Special provisions for vulnerable populations
42 USC 1396a includes special provisions that directly target vulnerable populations. For instance, it allows for disproportionate share payments that ensure certain facilities, such as those serving low-income or uninsured families, receive necessary financial support.
Additionally, Medicaid covers children under various programs, allowing for streamlined eligibility processes through Express Lane options. This approach aims to enhance access to care for children with disabilities or specific health conditions, ensuring they receive the necessary treatments and preventive services.
Waivers and modifications in state plans
Section 1396a (j) provides states with the option to apply for waivers, allowing them to bypass certain standard requirements. This flexibility can lead to innovative approaches to healthcare delivery tailored to local needs.
The implications of these waivers can be significant, fostering program innovations that potentially improve efficiency and accessibility. However, states must ensure they remain compliant with federal guidelines while exercising this flexibility.
State compliance and reporting requirements
States are bound by compliance obligations associated with 42 USC 1396a to ensure the transparent and accountable administration of Medicaid funds. This involves regular reporting and audits that uphold the integrity of the program.
Non-compliance can result in penalties or the loss of federal funding, which serves as a powerful incentive for states to maintain robust oversight mechanisms and to operate their Medicaid programs efficiently.
Changes and amendments to state plans over time
42 USC 1396a has undergone notable amendments that reflect the evolving landscape of healthcare needs and policies. These changes can have significant impacts on how states manage their Medicaid programs, introducing new services or altering eligibility standards.
States have established procedures for amending their plans in response to these legislative changes, which are crucial in adapting to the ever-changing healthcare environment.
The role of technology and documentation in 42 USC 1396a
The integration of technology into the management of documentation related to 42 USC 1396a is gaining momentum. States are leveraging digital tools to streamline processes, from plan submissions to beneficiary enrollment.
Platforms like pdfFiller offer powerful solutions for document creation, editing, and e-signing, empowering users to keep their documentation compliant and up to date, thus facilitating smoother state administration of Medicaid programs.
Best practices among states for implementing 42 USC 1396a
Across the nation, exemplary states have shared best practices for implementing their Medicaid programs under 42 USC 1396a. For instance, some states have focused on integrating community health services, which have bridged gaps in care accessibility.
Insights from these implementations provide valuable lessons for overcoming common challenges like funding limitations and administrative complexity, ultimately enhancing the quality and accessibility of medical assistance for all eligible individuals.
FAQs related to 42 USC 1396a state form
Understanding the intricacies of the 42 USC 1396a state form can raise several common questions. Individuals may inquire about the eligibility requirements, how to apply for Medicaid, and what processes are necessary to ensure compliance with federal guidelines.
Clarifications on common terms and policy language related to state plans can significantly aid users who are filling out forms or seeking assistance. Thus, familiarizing oneself with the nuances of these requirements is vital to effective navigation of the Medicaid landscape.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete 42 usc 1396a state online?
Can I create an electronic signature for signing my 42 usc 1396a state in Gmail?
How do I edit 42 usc 1396a state on an Android device?
What is 42 usc 1396a state?
Who is required to file 42 usc 1396a state?
How to fill out 42 usc 1396a state?
What is the purpose of 42 usc 1396a state?
What information must be reported on 42 usc 1396a state?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.