Get the free Blue Cross Anthem Prior Auth Form
Get, Create, Make and Sign blue cross anformm prior
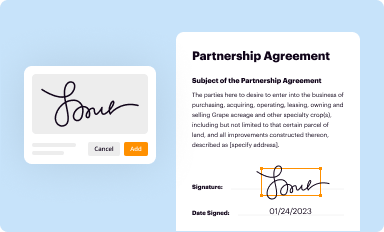
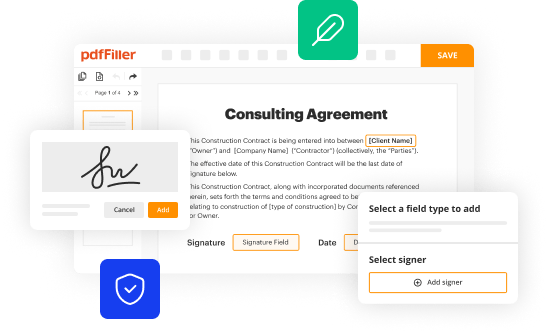
Editing blue cross anformm prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out blue cross anformm prior
How to fill out blue cross anformm prior
Who needs blue cross anformm prior?
Understanding the Blue Cross Anformm Prior Form: A Comprehensive Guide
Understanding the Blue Cross Anformm Prior Form
The Blue Cross Anformm Prior Form serves as a critical component of the healthcare process, designed to facilitate prior authorization for specific medical services and procedures. This form is essential for ensuring that necessary treatments are approved by insurance providers before they are administered, safeguarding both the patient’s health and the financial implications for the healthcare system. By requiring providers to submit this form, Blue Cross aims to maintain quality and efficacy in healthcare delivery.
The prior authorization process acts as a gatekeeper for planned medical services, ensuring that they meet established criteria for medical necessity and appropriateness. As healthcare costs continue to rise, the importance of effective prior authorization in managing these expenses cannot be overstated. This process encourages providers to justify the need for specific services, ultimately promoting patient safety.
Key features of the Blue Cross Anformm Prior Form
The Blue Cross Anformm Prior Form is specifically designed to outline the essential details necessary for obtaining prior authorization. Its purpose is twofold: to outline the specific services and treatments that require prior approval and to streamline communication between providers and Blue Cross. Understanding its key features can significantly enhance the efficiency of the authorization process.
Services commonly covered by the Blue Cross Anformm Prior Form include a variety of surgical procedures, certain medications, and specialized diagnostic tests. For instance, high-cost imaging procedures like MRIs and CT scans typically require prior authorization to ensure that they are medically necessary.
The primary users of this form include healthcare providers who submit requests on behalf of their patients and Blue Cross members themselves who may want to ensure compliance with their insurance plan. Understanding who uses the form can clarify the requirements and enhance the accuracy of submissions.
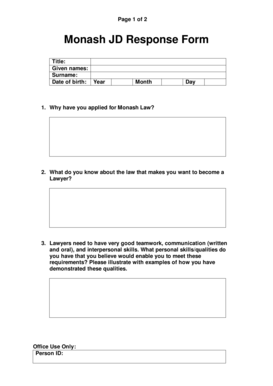
Step-by-step guide to filling out the Blue Cross Anformm Prior Form
Filling out the Blue Cross Anformm Prior Form accurately and completely is vital for ensuring timely approval. Here’s a comprehensive guide to help navigate the process.
Step 1: Gathering required information
Step 2: Completing the form
Ensure every section is filled out correctly. In the patient information section, double-check spellings and data accuracy. In the treatment description or procedure request section, it’s essential to specify the reason for the requested service clearly.
Step 3: Submission guidelines
Submit the form electronically, if available, to ensure prompt handling. Confirm which attachments are necessary, such as treatment plans or previous medical records, and avoid delays by ensuring all pertinent documents accompany the form.
Managing the prior authorization process
Once submitted, understanding how to manage the prior authorization process is essential. This includes tracking your submission and knowing what to expect during the waiting period.
Tracking your submission
Blue Cross offers a method to confirm receipt of your prior authorization request, typically via their online portal. You can also take note of the request number provided upon submission, which can be used for follow-ups.
What happens after submission?
After your submission, Blue Cross will review the request based on clinical guidelines. If additional information is needed, they will reach out directly to the provider. Effective communication between all parties is crucial during this phase.
Resources for support with the Blue Cross Anformm Prior Form
Accessing support is crucial when navigating the complexities of the Blue Cross Anformm Prior Form. Whether for additional inquiries or assistance with submissions, there are resources available.
Contact information for inquiries
Educational materials
Interactive tools available on pdfFiller
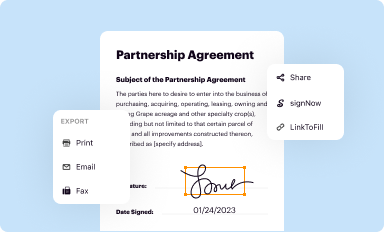
pdfFiller provides unique digital solutions that simplify the process of filling out the Blue Cross Anformm Prior Form. Users can utilize online editing features, which allow for straightforward form completion, and collaboration tools that aid in streamlining communication across healthcare teams.
Related forms and resources
Understanding the breadth of forms within the Blue Cross system can greatly assist in navigating prior authorization and claims processing. Familiarizing oneself with additional relevant forms ensures a comprehensive approach to healthcare management.
Accessing these forms can be quickly done through the pdfFiller platform, which offers comprehensive support for all Blue Cross members.
Staying informed about changes in the prior authorization process
Keeping abreast of any modifications to the prior authorization process via Blue Cross is vital for all stakeholders involved. Changes may arise due to regulatory shifts or internal policy updates.
Being proactive about identifying regulatory changes can enhance compliance and improve the overall management of the prior authorization process.
Frequently asked questions about the Blue Cross Anformm Prior Form
There are common queries that arise regarding the completion and management of the Blue Cross Anformm Prior Form that can help clarify uncertainties.
These FAQs serve as a valuable resource for both patients and providers in managing the intricacies of the Blue Cross Anformm Prior Form.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my blue cross anformm prior in Gmail?
How do I complete blue cross anformm prior online?
Can I create an eSignature for the blue cross anformm prior in Gmail?
What is blue cross anformm prior?
Who is required to file blue cross anformm prior?
How to fill out blue cross anformm prior?
What is the purpose of blue cross anformm prior?
What information must be reported on blue cross anformm prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.