
Get the free Sunshine Medicaid Prior Authorization Form
Get, Create, Make and Sign sunshine medicaid prior authorization
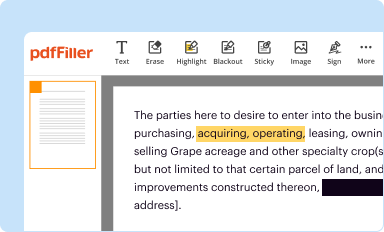
Editing sunshine medicaid prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out sunshine medicaid prior authorization
How to fill out sunshine medicaid prior authorization
Who needs sunshine medicaid prior authorization?
Understanding the Sunshine Medicaid Prior Authorization Form
Understanding the Sunshine Medicaid prior authorization form
The Sunshine Medicaid prior authorization form serves as a critical component in the Medicaid system, facilitating the approval of specific medical services, treatments, or prescription medications before they are administered or dispensed to patients. Essentially, prior authorization is a requirement set by insurers to ensure that certain procedures or drugs are medically necessary and covered by their health insurance plan.
This form plays a crucial role in the management of healthcare costs and quality of care. By requiring authorization, Medicaid can regulate the use of costly or non-evidence-based treatments, ensuring that patients receive only necessary healthcare services. The Sunshine Medicaid prior authorization form specifically outlines the required details about the patient's condition and the requested service, allowing for a streamlined review process.
Key components of the Sunshine Medicaid prior authorization form include fields for patient demographics, provider information, specific diagnosis codes, and a rationale for the requested service. Together, these elements help create a comprehensive view of the patient’s medical needs and the justification for the requested treatment.
Who needs the Sunshine Medicaid prior authorization form?
The Sunshine Medicaid prior authorization form is essential for both individuals seeking treatment under Medicaid and healthcare providers who administer care. To be eligible for prior authorization, individuals must be enrolled in the Sunshine Medicaid program, which caters primarily to low-income residents in specific regions. Providers, including hospitals, specialists, and pharmacies, must also participate in Medicaid and follow the guidelines outlined by the program to facilitate access to services for their patients.
Certain situations necessitate the completion of this form, particularly when patients require specific medical procedures, advanced imaging studies, or expensive prescription drugs. For instance, surgeries often require prior authorization to confirm their medical necessity. Prescription medications that fall outside the typical formulary may also require this form to ensure that they are being utilized appropriately.
Step-by-step guide to filling out the Sunshine Medicaid prior authorization form
Filling out the Sunshine Medicaid prior authorization form requires accurate and thorough documentation. The process begins by gathering the necessary information about the patient and provider. Key patient information includes full name, Medicaid ID number, date of birth, and contact details. Provider information should consist of the name, address, phone number, and NPI number of the healthcare provider overseeing the treatment.
A complete medical history and detailed treatment plan are also crucial components. This ensures that the request clearly articulates the medical necessity behind the services being sought. Once you have gathered all relevant documentation, you can proceed to fill out the form, which is typically divided into several sections.
Each section requires specific data:
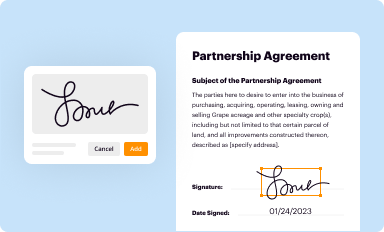
Common mistakes to avoid while filling out the form include incorrect patient or provider information, missing diagnosis codes, and inadequate rationale for the request. Once the form is completed, it’s essential to sign it properly. Electronic signature options are often available, and submission methods can vary from online uploads to mailing the form directly to the appropriate Medicaid office.
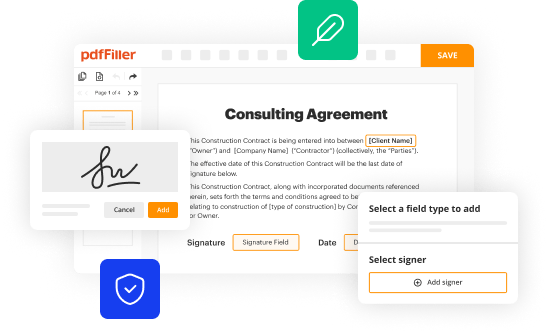
How to edit the Sunshine Medicaid prior authorization form online
Editing the Sunshine Medicaid prior authorization form online is made easier with tools like pdfFiller, which offers a user-friendly platform for document management. Users can upload their forms, fill in required information, and utilize various editing tools to ensure that every detail is precise and accurate.
One of the standout features of pdfFiller is its collaboration capacity, allowing healthcare providers and administrative teams to work together efficiently. This ensures that all aspects of the form are correct before submission, reducing the chances of errors that lead to delays or denials.
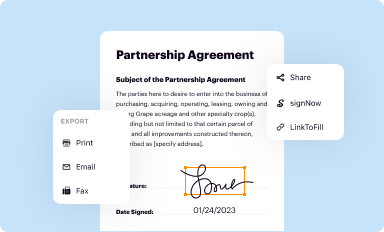
Once edits are complete, users can easily save their documents and store them securely on the cloud. This not only helps in maintaining a record of submissions but also allows for quick access should revisions or additional information be needed in the future.
Tracking your submission: What to expect after submission
After submitting the Sunshine Medicaid prior authorization form, it's crucial to understand what happens next. Typically, the request enters a review process where it is evaluated by Medicaid’s medical team. This might take several days or longer, depending on the complexity of the request and the volume of applications the office is handling.
Users can check the status of their authorization request through online portals or by contacting their Medicaid representative. Outcomes can vary, and it's important to be prepared for any of the following scenarios:
Frequently asked questions about the Sunshine Medicaid prior authorization form
Navigating the Sunshine Medicaid prior authorization form can lead to several common questions, particularly regarding timelines, resubmissions, and appeals. The typical processing time for a request varies, but most can expect a decision within 10 to 15 business days. For ongoing treatments, the form might need to be submitted regularly, depending on the specific guidelines set by Medicaid.
If a request is denied, it’s recommended to review the reason for denial provided by Medicaid. Often, additional supporting information or documentation can strengthen the case for approval upon resubmission.
Best practices for managing your Sunshine Medicaid prior authorization process
Staying organized is key to successfully managing the Sunshine Medicaid prior authorization process. One of the best practices is to maintain accurate records and documentation for every submission. This includes keeping copies of all authorization requests and the supporting documents provided. By having these records, it becomes much easier to address follow-ups and appeals if needed.
Effective communication also plays a significant role. Regularly communicating with healthcare providers and Medicaid representatives can provide clarity on requirements or changes in policy. Additionally, leveraging tools like pdfFiller can streamline document management, making it simpler to collaborate, edit, and track submissions from a single cloud-based platform.
Related documents and forms within the Medicaid landscape
The Sunshine Medicaid prior authorization form is part of a larger framework of documentation required by Medicaid systems. Understanding other important Medicaid forms, such as the Medicaid application form, the Medicaid re-certification form, and the appeals process, can enhance your ability to navigate the healthcare landscape effectively.
These forms interrelate with the prior authorization process by establishing eligibility, ensuring compliance, and facilitating ongoing access to necessary treatments. Familiarity with these documents allows individuals to be better prepared and informed, ensuring a smoother experience throughout their healthcare journey.
Empowering your healthcare journey with pdfFiller
Utilizing pdfFiller to manage the Sunshine Medicaid prior authorization process brings numerous advantages. Users can edit, sign, and collaborate on the form conveniently, ensuring all submissions are accurate and timely. The platform's streamlined workflow reduces the headaches often associated with paperwork, particularly in the intricate landscape of healthcare documentation.
User testimonials highlight the platform’s effectiveness: many have successfully navigated the complex authorization process using pdfFiller, allowing them to focus on what truly matters — their health and well-being.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete sunshine medicaid prior authorization online?
How do I edit sunshine medicaid prior authorization straight from my smartphone?
How do I fill out sunshine medicaid prior authorization using my mobile device?
What is sunshine medicaid prior authorization?
Who is required to file sunshine medicaid prior authorization?
How to fill out sunshine medicaid prior authorization?
What is the purpose of sunshine medicaid prior authorization?
What information must be reported on sunshine medicaid prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.















