Get the free hmo-exchange-prior-authorization-criteria-en.pdf
Get, Create, Make and Sign hmo-exchange-prior-authorization-criteria-enpdf
How to edit hmo-exchange-prior-authorization-criteria-enpdf online
Uncompromising security for your PDF editing and eSignature needs
How to fill out hmo-exchange-prior-authorization-criteria-enpdf
How to fill out hmo-exchange-prior-authorization-criteria-enpdf
Who needs hmo-exchange-prior-authorization-criteria-enpdf?
HMO Exchange Prior Authorization Criteria ePDF Form: A Comprehensive Guide
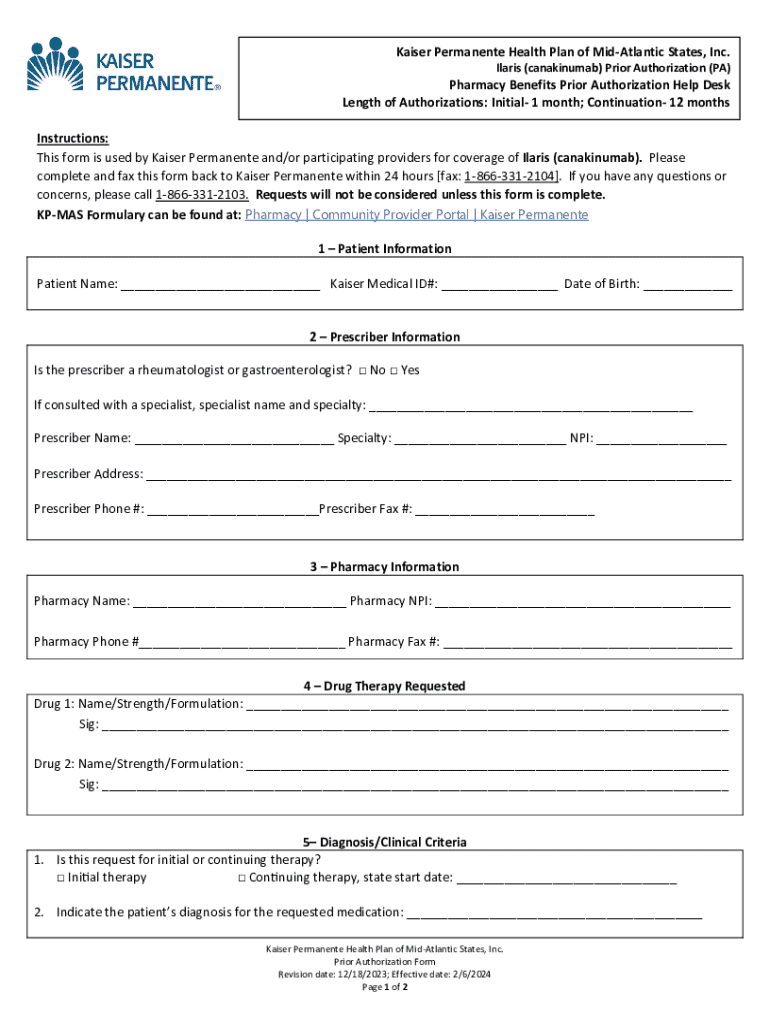
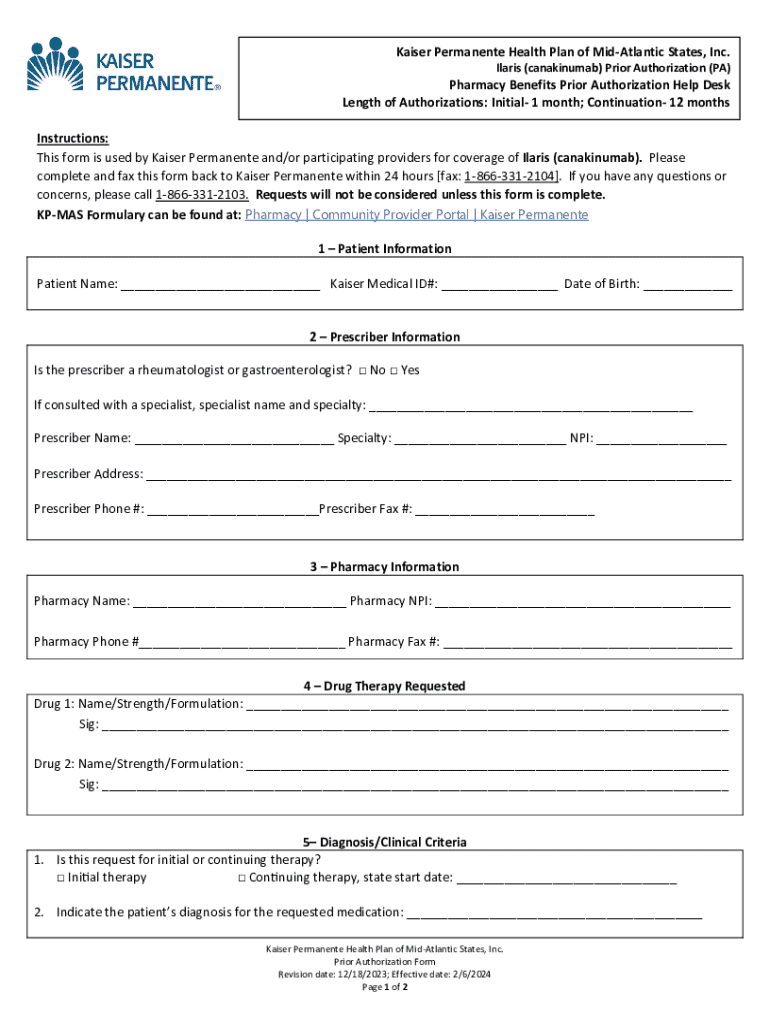
Overview of prior authorization in HMO exchange
Prior authorization is a crucial component of the healthcare managed care system, particularly in Health Maintenance Organizations (HMOs). It refers to the requirement that healthcare providers obtain approval from a health insurance plan before delivering a specific service, procedure, or medication to a patient. This step is essential to ensure that the service aligns with clinical guidelines and is deemed necessary for the patient’s medical condition.
The importance of prior authorization cannot be overstated. It serves as a mechanism to manage costs and ensure appropriate healthcare use, while also safeguarding patients from unnecessary procedures. By requiring prior authorization, insurers can prevent misuse of medical resources, keep premiums lower, and maintain overall quality of care.
How prior authorization works can vary across different HMOs. Typically, the process involves a provider submitting a request for authorization detailing the patient's condition and the necessity of the proposed treatment. Patients benefit from this process as it fosters a collaborative approach between them and healthcare providers, ensuring that treatments meet predefined standards of care.
Understanding the HMO exchange prior authorization criteria
Navigating the HMO exchange prior authorization criteria requires a clear understanding of what services typically necessitate this approval. Authorization criteria serve as guidelines that help determine the medical necessity of procedures, ensuring that they align with best practices and standards.
Common medical procedures that often require prior authorization include surgeries, advanced imaging studies, and referrals to specialists. Similarly, behavioral health services such as inpatient treatment for mental health conditions typically demand authorization due to the complexity involved in these types of care.
Additionally, certain prescription medications can also be subject to prior authorization. This stipulation often arises with high-cost or specialty drugs, where it is necessary to assess the appropriateness of the medication relative to alternative treatments. It’s worth noting that criteria can vary significantly between different health plans, making it essential for providers to understand the specific requirements tied to their particular HMO.
How to use the HMO exchange prior authorization ePDF form
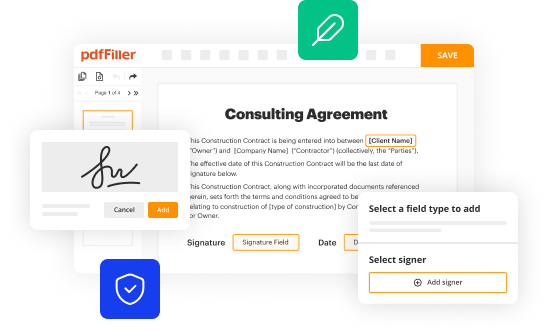
The HMO exchange prior authorization ePDF form is a critical tool for both healthcare providers and patients. It is designed to make the submission process smoother and more efficient. Features such as interactive fields and built-in checklists make it user-friendly and enhance compliance with submission requirements.
To effectively utilize the ePDF form, follow these step-by-step instructions:
Tips for successful submission of the prior authorization form
Completing the HMO exchange prior authorization form accurately is crucial for a swift approval process. Here are best practices to enhance your submission’s success rate:
Common mistakes include providing incomplete patient information, failing to include necessary documentation, and misunderstanding the criteria for specific services. To mitigate such errors, consider utilizing pdfFiller’s interactive features that simplify the process.
Tracking the status of your prior authorization request
Once a submission is made, tracking the status of your HMO exchange prior authorization request is essential for both providers and patients. With pdfFiller, users can conveniently monitor submissions through the platform, receiving timely updates on their requests.
It's important to understand the typical review process and what to expect during the authorization period. Generally, insurers undertake reviews of prior authorization requests promptly, with turnaround times varying by service type and urgency level. Regular notifications will be sent, providing updates on the request's status.
Understanding denials and appeals
Denials of prior authorization requests can be frustrating, but understanding the reasons behind these denials is vital for effective appeals. Common reasons include insufficient documentation, failure to satisfy medical necessity criteria, and incomplete forms.
If a request is denied, the appeal process must be initiated promptly to avoid delays in care. To appeal a denial, it’s essential to gather comprehensive documentation that supports the necessity of the proposed treatment or service. The required documentation often includes clinical notes, test results, and any previous authorizations.
Additional resources for stakeholders
Support during the prior authorization process is crucial for healthcare providers. Several resources are available to aid stakeholders in understanding and navigating this complex landscape. Comprehensive guides can offer step-by-step assistance tailored to the specific requirements of various HMOs.
Additionally, accessing provider networks and verifying eligibility details through the HMO exchange helps ensure compliance with coverage requirements. Frequently asked questions (FAQs) sections dedicated to prior authorization can also clarify common uncertainties faced by providers and patients alike, thereby fostering smoother interactions.
Tools and features of pdfFiller for document management
pdfFiller provides a robust array of tools designed for efficient document management, ensuring users can create, edit, and manage their healthcare documents seamlessly. This platform allows users to eSign documents, collaborate with teams, and enjoy cloud-based access and storage, making document handling more convenient.
With features tailored specifically to streamline the prior authorization process, pdfFiller empowers users to navigate paperwork with ease. The removal of traditional barriers such as physical paperwork and the correspondence delays associated with postal services means that healthcare providers and patients can focus on what truly matters—delivering and receiving timely healthcare.
Related topics and forms
For healthcare professionals and stakeholders involved in the prior authorization process, understanding related documentation can enhance overall efficiency. Forms such as precertification requests and coverage guidelines are also integral in pairing with the HMO exchange prior authorization criteria.
Within pdfFiller, additional ePDF forms can be accessed to further streamline healthcare management processes. Therefore, understanding how these related forms interconnect can improve the handling of standards and protocols governing patient care.
The importance of staying updated
Staying informed about changes in prior authorization criteria is critical for both healthcare providers and patients. Changes can arise due to new policies, updated guidelines, or shifts in healthcare regulations. Utilizing pdfFiller tools can enable users to set alerts for updates, ensuring that they remain informed and adaptable.
Continuous learning through courses, webinars, and updates about prior authorization best practices enhances compliance and workflow. This proactive approach is beneficial for managing successful patient outcomes while navigating the complexities of healthcare documentation.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify hmo-exchange-prior-authorization-criteria-enpdf without leaving Google Drive?
How do I execute hmo-exchange-prior-authorization-criteria-enpdf online?
How do I make changes in hmo-exchange-prior-authorization-criteria-enpdf?
What is hmo-exchange-prior-authorization-criteria-enpdf?
Who is required to file hmo-exchange-prior-authorization-criteria-enpdf?
How to fill out hmo-exchange-prior-authorization-criteria-enpdf?
What is the purpose of hmo-exchange-prior-authorization-criteria-enpdf?
What information must be reported on hmo-exchange-prior-authorization-criteria-enpdf?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.