Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form



Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
Your Complete Guide to the Prior Authorization Request Form
Understanding the prior authorization request form
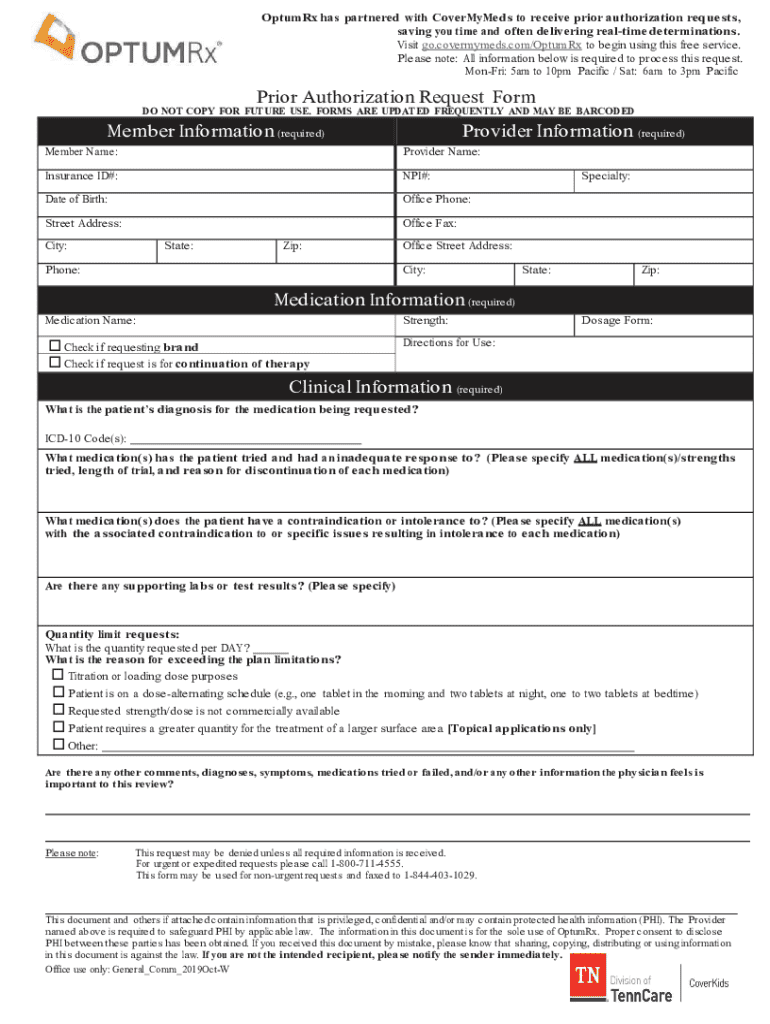
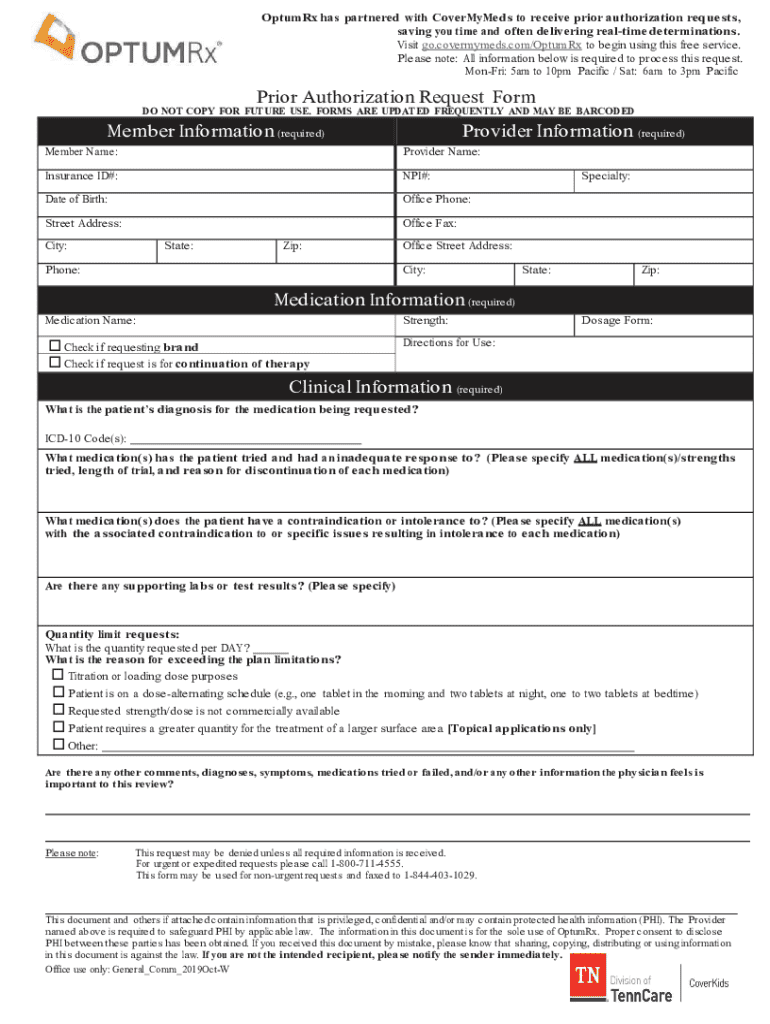
A prior authorization request form is a critical document in the healthcare landscape, designed to streamline the approval of certain medical services, procedures, and medications by insurance companies before they are provided to patients. Understanding this form is essential because it serves as a gatekeeper that ensures medical necessity and cost-effectiveness, ultimately influencing approval for various treatments. Common scenarios necessitating a prior authorization request include specialized procedures like MRIs, certain medications—notably high-cost drugs—and advanced treatments that exceed standard guidelines.
Primarily, these forms are utilized by patients who require medical services, healthcare providers who deliver these services, and insurance companies that manage patient care. The involvement of all three parties illustrates the collaborative nature of healthcare, where clear communication and adherence to protocols can enhance patient outcomes.
Key components of the prior authorization request form
Filling out a prior authorization request form involves providing essential information that assures the insurance company of the medical necessity of the requested procedure or treatment. The form is typically structured to gather critical patient details, including
Additionally, the insurance information section must detail payer-specific requirements. This part of the form is vital because missing or incomplete information can lead to common mistakes, such as delayed approvals or outright denials. To ensure a smooth process, double-check the guidelines provided by the insurance carrier before submitting the form.
Step-by-step guide to completing the form
Completing the prior authorization request form requires preparation and attention to detail. Start by gathering necessary documents that support the treatment request, which may include test results, referral letters, and relevant medical history. Here’s a step-by-step guide to assist you:
While filling the form, prioritize clarity and accuracy. It's often recommended to use typed inputs for legibility, as handwritten responses can lead to misunderstandings.
Editing and customizing your form
Once the prior authorization request form is filled out, the next step involves refining and customizing the document to adhere to specific insurance requirements. pdfFiller provides vital editing tools that help in this area. Users can access editing features that allow for text adjustments, checkbox selections, and even the addition of comments. By utilizing pdfFiller’s capabilities, you can ensure that your form is tailored and accurate per your insurance provider’s specifications.
Moreover, eSigning options are available, which provide an essential feature for consent and authentication. Digital signatures can expedite the submission process and facilitate quicker responses from insurance carriers, ensuring that your requests get prompted faster.
Submitting the prior authorization request form
Submitting the completed prior authorization request form can be done through various methods. Electronic submission is the most efficient, allowing you to send the form directly to the insurance provider's designated portal, which usually speeds up the review process. If mailing the form is necessary, ensure you use a reliable delivery service and obtain a tracking number to confirm receipt.
Once submitted, it’s wise to follow up on the status of your submission. Many insurance companies provide a reference number upon submission, which you can use to track your request. Understanding potential outcomes is equally crucial; requests may be approved, denied, or require additional information. Knowing the expected timelines can help you remain informed throughout the process.
Managing the prior authorization process
Receiving a denial for a prior authorization request can be a disheartening experience, but it is not the end of the road. Understanding the denial letters issued by insurance companies is crucial, as they often outline reasons for the denial and steps for appealing the decision. Your next steps should include gathering any necessary documentation that supports an appeal, clearly outlining the medical necessity of the requested treatment, and resubmitting your appeal promptly.
Effective communication with insurance providers during this phase can significantly enhance your chances of a successful appeal. Prepare a list of pertinent questions and any supporting evidence you have to facilitate a productive conversation with the insurer.
Interactive tools and resources
For users looking to streamline their experience with prior authorization requests, pdfFiller offers several features tailored specifically for this process. Accessing pre-filled templates can save time, while collaborative features enable teams to review documents together seamlessly. These tools are not just user-friendly; they are also designed to minimize errors and ensure the accuracy of submissions.
Within the platform, you can find an FAQ section that addresses common questions about the prior authorization request process, providing immediate assistance and guidance.
Best practices for future submissions
Staying organized and managing your documentation effectively is essential for handling prior authorization requests. Develop a systematic approach to store and organize your authorization requests, ensuring easy access when new forms are required. Furthermore, remaining informed about insurance policy changes is crucial; insurers may update their requirements frequently, and staying abreast of these shifts will streamline your future submissions.
Troubleshooting common issues
Common mistakes in prior authorization requests can lead to denials or delays. Avoid these frequent errors, such as incomplete sections, misentered information, or unclear treatment descriptions. If you encounter persistent issues, contacting support teams within the insurance company can provide valuable guidance and rectify mistakes quickly.
When reaching out for additional help, come prepared with important details about your request, including dates and names of previous interactions. This preparation will enhance the effectiveness of your communication and expedite the problem resolution process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in prior authorization request form without leaving Chrome?
Can I sign the prior authorization request form electronically in Chrome?
How do I fill out the prior authorization request form form on my smartphone?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.