Get the free Tricare Prior Authorization Request Form for Semaglutide Injection (wegovy), Tirzepa...
Get, Create, Make and Sign tricare prior authorization request



How to edit tricare prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out tricare prior authorization request

How to fill out tricare prior authorization request
Who needs tricare prior authorization request?
Comprehensive Guide to Tricare Prior Authorization Request Form
Understanding Tricare and its importance
Tricare is the health care program for military service members, retirees, and their families, providing comprehensive health care benefits. It is designed to offer a range of medical services, including preventive, acute, and specialty care. Understanding the intricacies of Tricare is crucial for beneficiaries to maximize the benefits available to them.
Prior authorization plays a vital role in the Tricare system, ensuring that the medical services are deemed medically necessary before they are provided. This pre-approval step helps control health care costs, curtails unnecessary procedures, and promotes effective treatment. For beneficiaries, understanding this process means accessing care efficiently while avoiding unexpected expenses.
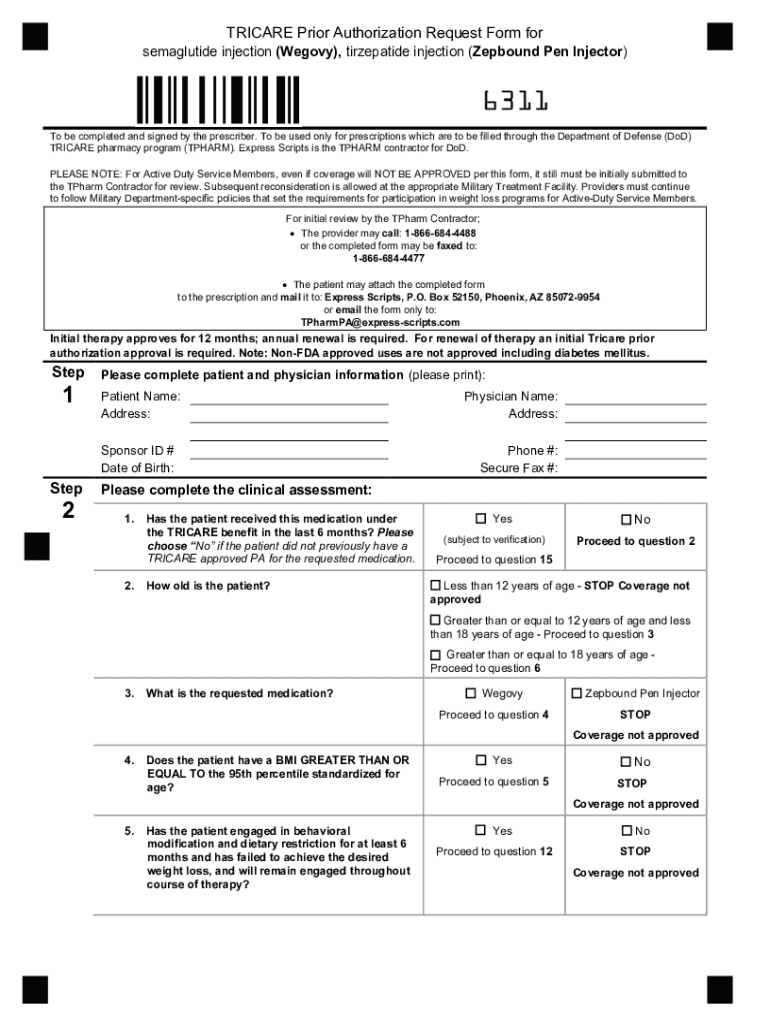
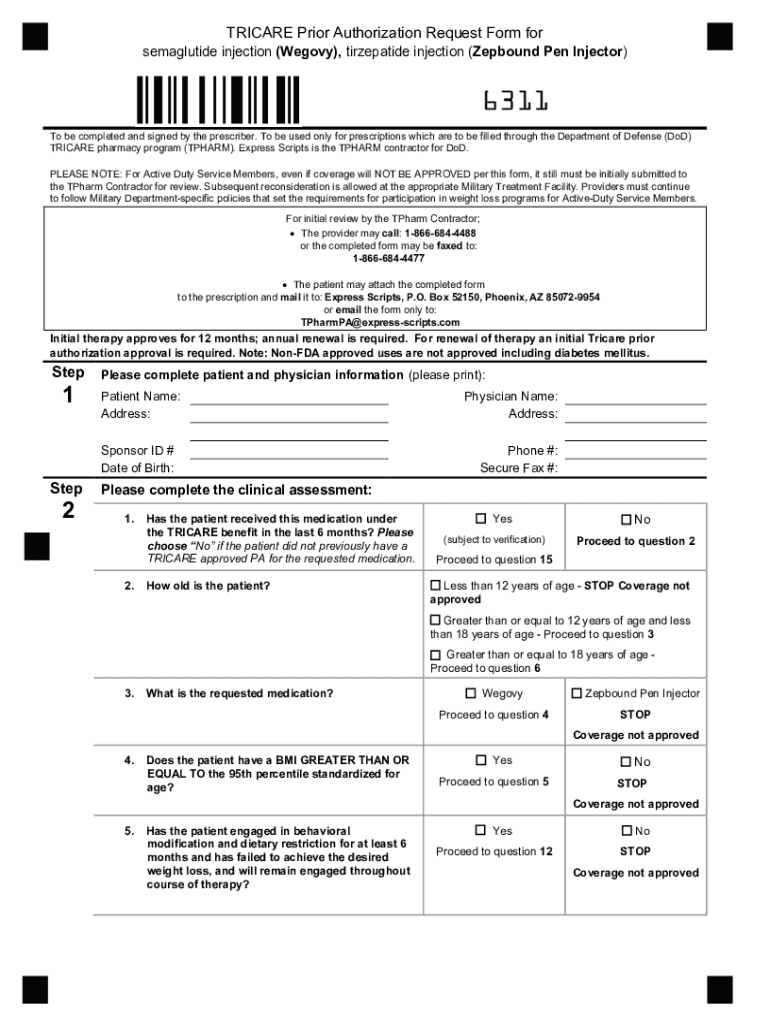
What is the Tricare prior authorization request form?
The Tricare prior authorization request form is a critical document required for certain medical procedures, tests, or prescriptions to receive approval from Tricare before the service can be utilized. The main purpose of the form is to gather pertinent information regarding the patient’s medical condition and justify the necessity of the requested service.
To submit a prior authorization request, a beneficiary or provider must meet specific eligibility requirements. Typically, these requirements include having active Tricare coverage and ensuring that the requested care falls under services that necessitate prior approval. Understanding the approval process can help avoid delays in receiving necessary medical treatments.
Who needs to use the Tricare prior authorization request form?
The Tricare prior authorization request form is essential for various parties involved in the process of healthcare management. Healthcare providers often recommend submitting an authorization request when a patient requires specialized services or expensive treatments. It is crucial for providers to understand the specific scenarios in which an authorization is necessary, as this can greatly influence patient care timelines.
Beneficiaries must also grasp their responsibilities regarding prior authorization. It is essential to communicate effectively with healthcare providers and ensure documentation is complete. Certain cases, such as for children, mental health services, or high-cost treatments, may have unique requirements or nuances that necessitate further understanding.
Detailed breakdown of the Tricare prior authorization request form
Filling out the Tricare prior authorization request form accurately is critical for securing timely approvals. The form consists of several essential sections, each requiring precise information to avoid delays. Below is a breakdown of each section that must be completed when submitting the form.
Common mistakes can lead to delays in the approval process. Failing to provide adequate medical justification or neglecting to include essential patient information could result in a denial or prolonged review period, which can affect patient care.
How to effectively submit the Tricare prior authorization request form
Submitting the Tricare prior authorization request form can be done through various methods. Beneficiaries and healthcare providers can choose from online submission, traditional mail, or fax. Online channels are typically faster, ensuring the request reaches Tricare quickly and allows for tracking submission status.
Regardless of the method selected, certain best practices should be followed. Ensure that all sections of the form are filled out completely and accurately to avoid unnecessary delays. After submission, beneficiaries should be aware of the review timeline, which may differ based on the type of request. Notifications of approval or denial are usually communicated via the chosen submission method.
Modifications and follow-ups
Modifications to a submitted Tricare prior authorization request can occur when new information arises or if initial documentation was insufficient. It is important to understand the circumstances under which modifications can be made and how to proceed with them effectively. This may involve completing a new form or providing supplementary documentation.
In cases where a request is denied, beneficiaries have the right to initiate an appeal. The appeal process includes submitting a letter that outlines reasons for the appeal, along with any relevant supporting evidence. It is crucial to be diligent and prepared with all necessary documentation to strengthen the appeal and improve the chances of overturning the denial.
Frequently asked questions about Tricare prior authorization
There are many common inquiries regarding the Tricare prior authorization process that can cause confusion for both providers and beneficiaries. Understanding these questions can help navigate the system more effectively and with greater confidence.
Tools and resources for managing your authorization requests
Efficiency in completing and managing the Tricare prior authorization request form can be greatly enhanced using dedicated tools. One such example is pdfFiller, which empowers users to seamlessly edit PDFs, eSign, and manage their documents all from a single, cloud-based platform. This can significantly reduce errors and ensure that all documents remain organized.
Using pdfFiller can simplify the process of filling out forms and managing submissions. Interactive tools are available that guide users through each step of the process, making it a practical choice for both individual beneficiaries and healthcare teams.
Staying updated with Tricare policies and changes
The landscape of health care can evolve rapidly, and staying informed about Tricare policies is vital for both beneficiaries and providers. Regularly checking official Tricare communications, including announcements, newsletters, and policy updates, is essential to understand any changes that could affect service availability or authorization requirements.
Engaging with community forums and support groups can also provide valuable insights and peer support. By sharing experiences and gaining knowledge from others, beneficiaries and providers can navigate the complexities of the TriCare system more confidently.
Final thoughts on navigating Tricare prior authorizations
Navigating the Tricare prior authorization request form can seem overwhelming, but with the right tools and knowledge, beneficiaries can enhance their experience significantly. Open communication between healthcare providers and patients is essential to understanding what is required for successful authorizations.
Utilizing resources like pdfFiller for document management can streamline the process and alleviate some of the stress associated with paperwork. Remember, informed patience is a key ingredient to successfully managing your health care needs through the Tricare system.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit tricare prior authorization request online?
Can I create an electronic signature for signing my tricare prior authorization request in Gmail?
How do I complete tricare prior authorization request on an Android device?
What is tricare prior authorization request?
Who is required to file tricare prior authorization request?
How to fill out tricare prior authorization request?
What is the purpose of tricare prior authorization request?
What information must be reported on tricare prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.