Get the free Motegrity (prucalopride) Prior Authorization Request Form
Get, Create, Make and Sign motegrity prucalopride prior authorization



How to edit motegrity prucalopride prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out motegrity prucalopride prior authorization

How to fill out motegrity prucalopride prior authorization
Who needs motegrity prucalopride prior authorization?
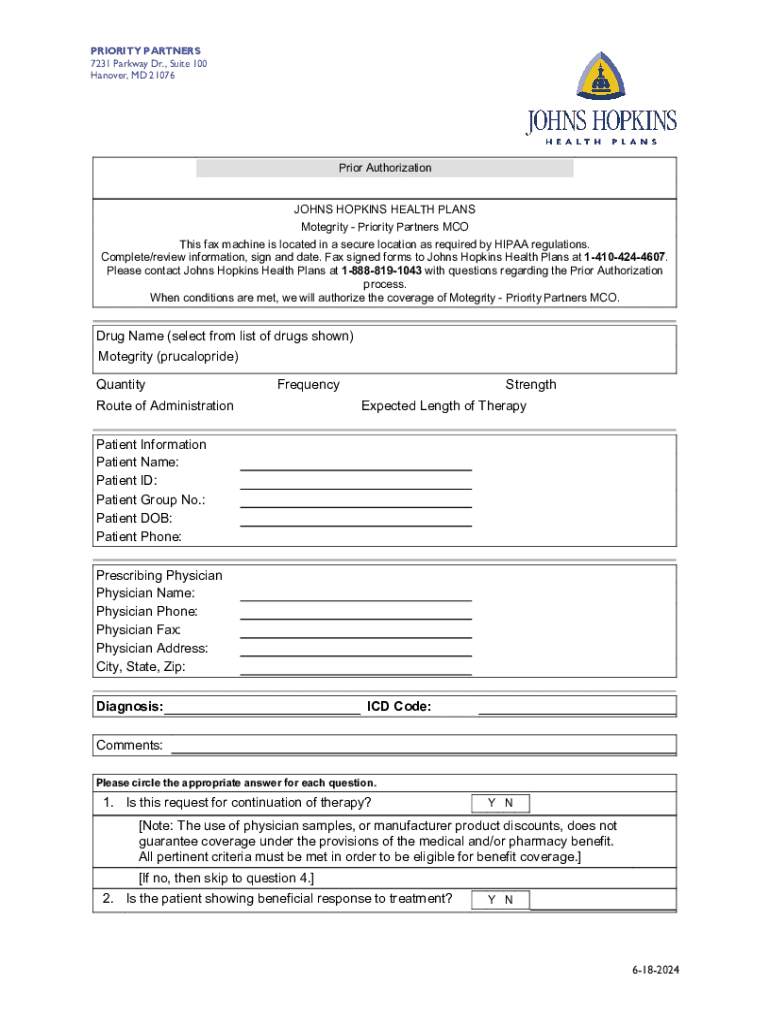
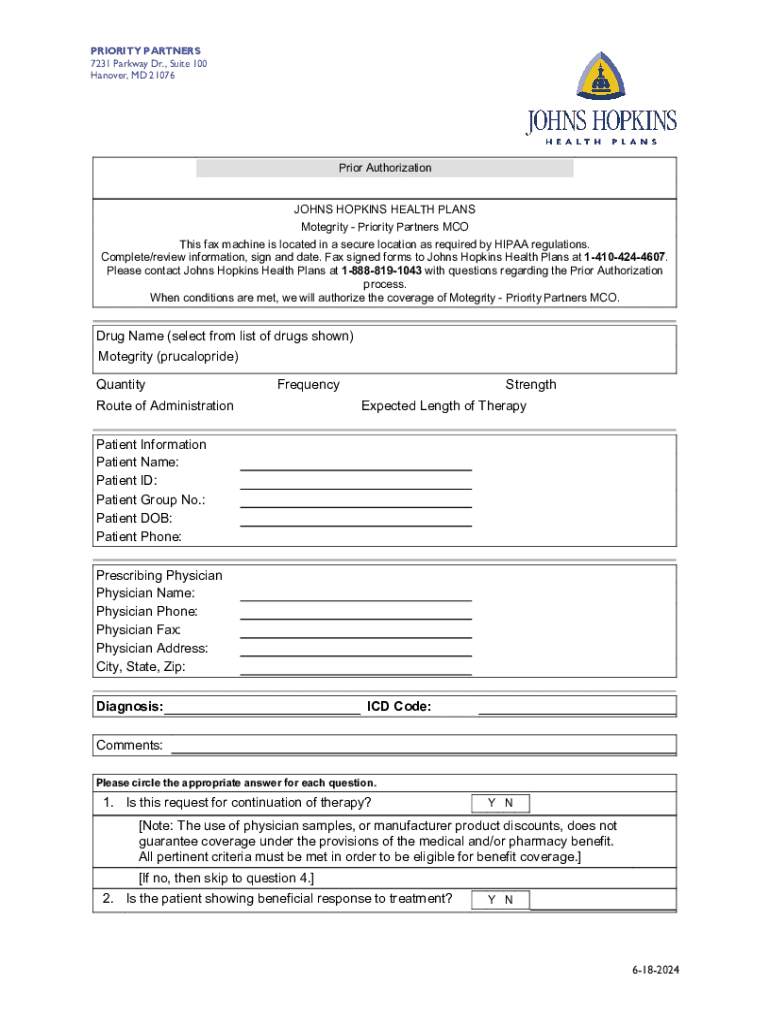
Understanding the Motegrity Prucalopride Prior Authorization Form
Understanding Motegrity (Prucalopride)
Motegrity, known generically as prucalopride, is a selective serotonin receptor agonist primarily used to treat chronic constipation in adults. It works by enhancing gastrointestinal motility and facilitating bowel movements, making it beneficial for patients who do not respond adequately to laxatives. Its efficacy can significantly improve quality of life by alleviating the discomfort associated with constipation.
Before a patient can access Motegrity through their insurance, prior authorization is often mandated. This process ensures that the medication is medically necessary for the patient’s treatment plan, thereby aligning with the insurance provider’s guidelines. Understanding the prior authorization process is crucial for both healthcare providers and patients to ensure smooth access to necessary medications.
The need for a prior authorization form
Insurance companies require prior authorization for multiple reasons, including cost containment and ensuring appropriate use of high-cost medications. This step helps to manage healthcare expenses and promotes patient safety by confirming that prescribed therapies are suitable given the patient's medical history.
However, this requirement can impact patient care by creating delays in treatment initiation. Furthermore, challenges such as obtaining the necessary documentation or misunderstandings regarding the criteria for approval can complicate the process. Health professionals often encounter frustrations when navigating these requirements, potentially hindering patient outcomes.
Key components of the Motegrity prior authorization form
The Motegrity prucalopride prior authorization form typically includes several critical components. Firstly, the form requires detailed patient information, including personal details such as the patient’s name, date of birth, and insurance provider. Additionally, it collects information about the patient's medical history as it relates to chronic constipation, which is essential for the authorization process.
Moreover, the prescribing physician's information, including their credentials and contact details, must be included. This section often features a detailed description of previous treatments attempted, such as laxatives or other therapies, to showcase that Motegrity is a necessary step in the treatment regimen. Lastly, the form should specify the prescribed dosage, administration schedule, and an anticipated duration of treatment.
Step-by-step guide to completing the Motegrity prior authorization form
Completing the Motegrity prucalopride prior authorization form can be streamlined by following these steps. Start by gathering all necessary documentation, including medical records and previous authorization letters, which will aid in supporting the request. Next, fill in the patient information, ensuring all details are accurate and current to avoid processing delays.
Continuing, the medical history and treatment details must be comprehensive, outlining past medication attempts and responses. After filling out the form, review all the information carefully to confirm accuracy and completeness. Finally, submit the form through the appropriate channels, whether that’s via fax or an online portal, ensuring you follow correct submission procedures.
Common mistakes to avoid when submitting a prior authorization form
Submitting a valid Motegrity prucalopride prior authorization form requires attention to detail. One common pitfall is failing to provide complete or accurate information, which can delay the authorization process. Additionally, neglecting to attach necessary supporting documents often leads to rejection of the request on the first attempt.
Other frequent mistakes include delayed submissions and not being aware of any specific preconditions set by insurance providers. It's essential to engage with healthcare providers to clarify requirements and ensure timely processing, thus avoiding unnecessary setbacks in medication access.
Tracking the status of your prior authorization request
Once the Motegrity prucalopride prior authorization form is submitted, tracking the request is vital for a timely response. Healthcare providers and patients can follow up on submitted requests, either through direct contact with the insurer or by utilizing online portal features when available.
Typically, waiting periods for prior authorization decisions can vary, so patience is essential. If a request is denied, understanding the reasons for denial is critical; this often requires engaging in an appeal process. Patients and providers should prepare to submit additional information or clarification to support the case for approval.
Utilizing pdfFiller for your Motegrity prior authorization form
pdfFiller presents a powerful solution for managing the Motegrity prucalopride prior authorization form. With its cloud-based platform, users can easily edit, sign, and store documents. One significant advantage of using pdfFiller is that it allows for seamless collaboration between healthcare teams and patients, ensuring everyone involved in the treatment process is well-informed and aligned.
The platform also provides interactive tools to streamline submission processes. With mobile accessibility, users can manage their authorization requests on the go, ensuring that important deadlines are met, and the required follow-ups are conducted appropriately.
Frequently asked questions (FAQs)
Patients and providers often have questions regarding the Motegrity prucalopride prior authorization form and its process. One common inquiry involves what steps to take if an insurance provider denies coverage. It is crucial to appeal the decision, ensuring that all necessary documentation and a clear rationale for medical necessity are included in the appeal.
Another frequent question centers around the typical duration of the prior authorization process. This can vary significantly based on the insurer’s guidelines and the complexity of the case. Patients may wonder if there’s a way to expedite the authorization request, which is sometimes possible depending on the urgency of the medical condition.
Additional tips for a smooth prior authorization experience
Building a strong case for authorization is essential when completing the Motegrity prucalopride prior authorization form. Effective communication with healthcare providers and insurers can facilitate clarity and expedite the process. Furthermore, engaging in patient advocacy can ensure that individuals receive the treatment they need in a timely manner.
It’s beneficial for patients and providers to maintain organized records of all communications and submissions related to the authorization process. This level of detail can enhance follow-up interactions and help form stronger arguments for appeals if they become necessary.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete motegrity prucalopride prior authorization online?
Can I create an electronic signature for the motegrity prucalopride prior authorization in Chrome?
How do I fill out motegrity prucalopride prior authorization on an Android device?
What is motegrity prucalopride prior authorization?
Who is required to file motegrity prucalopride prior authorization?
How to fill out motegrity prucalopride prior authorization?
What is the purpose of motegrity prucalopride prior authorization?
What information must be reported on motegrity prucalopride prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.