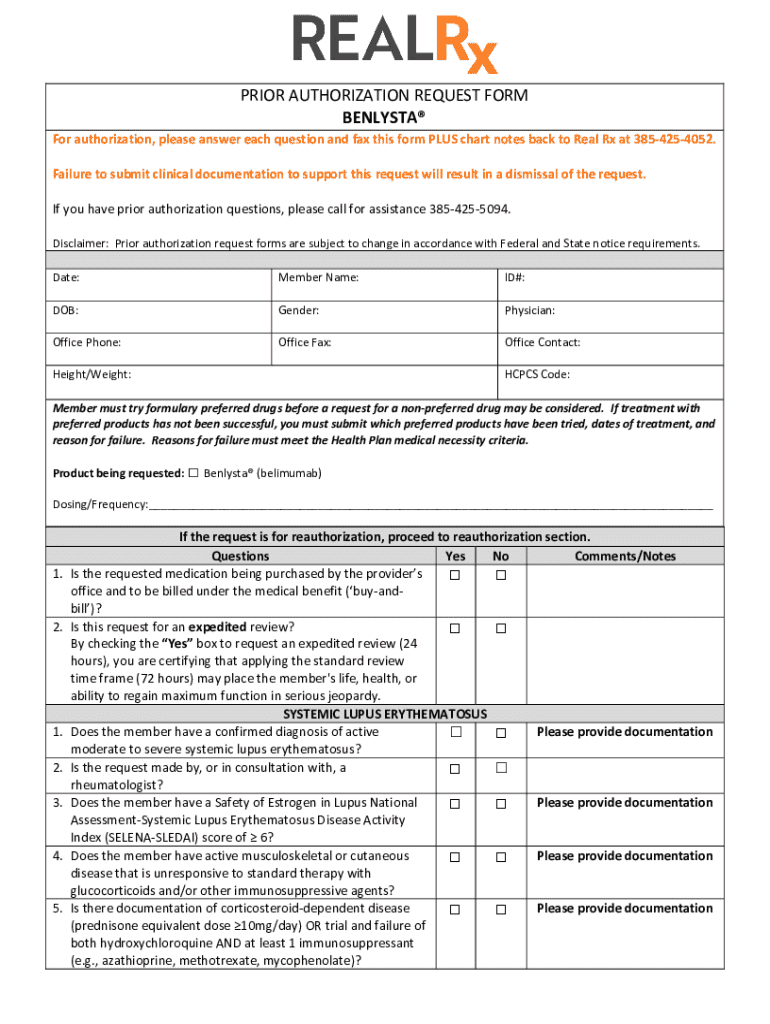
Get the free PRIOR AUTHORIZATION REQUEST FORM ®
Get, Create, Make and Sign prior authorization request form



How to edit prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
A comprehensive guide to the prior authorization request form
Understanding prior authorization
Prior authorization is a process used by health insurance companies to determine if they will cover a prescribed procedure, service, or medication. This process is crucial in managing costs and ensuring that prescribed treatments are medically necessary.
The importance of prior authorization in healthcare cannot be overstated. It serves to ensure the cost-effectiveness of healthcare services while also promoting patient safety by allowing medical providers to review treatment options thoroughly.
Overview of the prior authorization request form
The prior authorization request form serves as a formal document submitted by healthcare providers to insurance companies, outlining the necessity of a treatment or service. It acts as an essential tool in the approval process.
Key components of the form include:
Forms may vary across different providers and insurers, often differing in required information and formatting. It's vital to use the correct version familiar with the specific insurance provider.
Steps to fill out the prior authorization request form
To ensure a smooth authorization process, it's essential to gather necessary information before filling out the form. Start by compiling relevant medical history that supports the treatment requested.
When completing the form, focus on these sections:
After trying to complete all sections, review your submission carefully to identify common pitfalls, such as missing information or unclear justification.
Editing and customizing your prior authorization request form
Before submitting, making edits and customizations to the prior authorization request form is crucial. Various tools are available for editing, including online PDF editors that allow for easy manipulation of the document.
pdfFiller offers features to simplify these edits. With its tools, you can:
Ensuring compliance with insurance standards is paramount. Double-check that all completed information aligns with the requirements stipulated by the insurance provider.
Submitting the prior authorization request form
Once the form is filled out correctly, it must be submitted according to the insurance company’s guidelines. There are several methods of submission available to medical providers:
After submission, following up is critical. Recommended practices include documenting the submission date and contacting the insurance provider to confirm receipt and inquire about the response timeline. If your request is denied, you should be prepared to appeal the decision.
Collaborative efforts in managing the authorization process
Collaboration among healthcare teams is essential in facilitating the authorization process effectively. Involving various stakeholders, including administrative staff, can aid in ensuring every part of the request is appropriately completed.
Real-time edits allowed by pdfFiller enhance the transparency and efficiency of the entire process.
Challenges in prior authorization and how to overcome them
The prior authorization process often faces challenges, including delays and outright denials. Understanding the common reasons for these issues can help mitigate frustrations.
Overcoming these challenges often requires a proactive approach combined with effective use of available technologies.
FAQs about the prior authorization request form
When engaging with the prior authorization process, understanding potential outcomes is vital. Here are common questions that arise:
Additional support for users of the prior authorization request form
Healthcare providers and patients alike may need support while navigating the complexities of the prior authorization process. Access to timely assistance is essential.
Popular links related to prior authorization
To further enhance your understanding and manage the prior authorization request form, access to additional resources is key. Here are popular links that can aid your journey:






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out the prior authorization request form form on my smartphone?
How can I fill out prior authorization request form on an iOS device?
How do I complete prior authorization request form on an Android device?
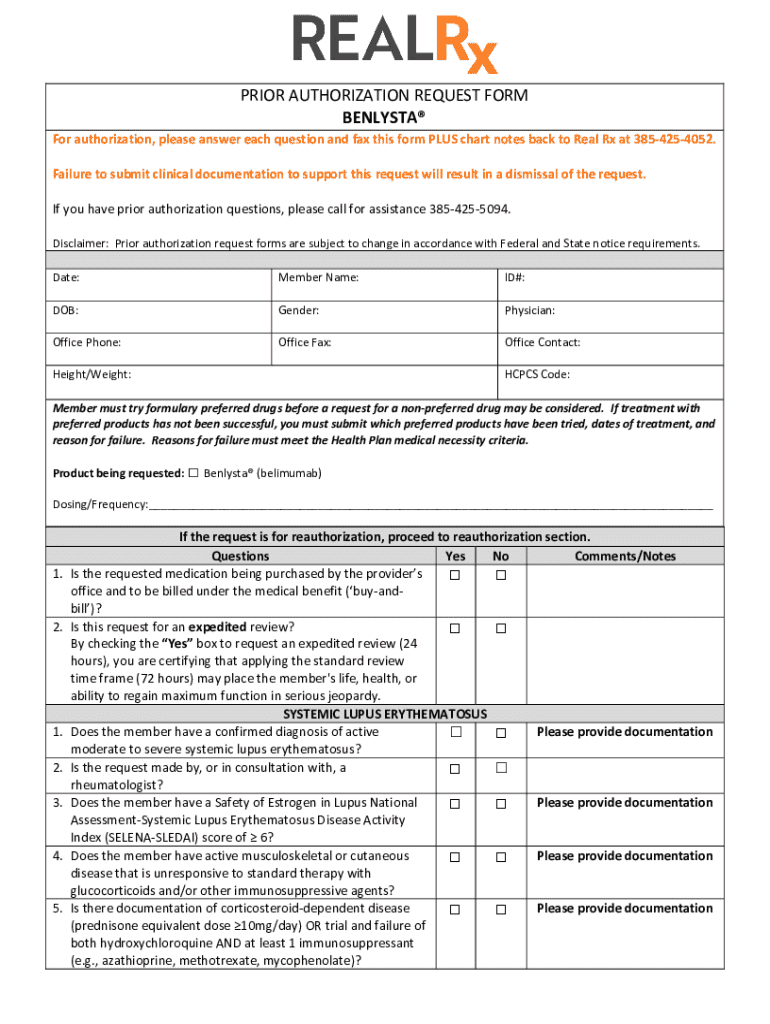
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.