Get the free yescarta denied by insurance
Get, Create, Make and Sign yescarta insurance denial form
How to edit yescarta denied by insurance online
Uncompromising security for your PDF editing and eSignature needs
How to fill out yescarta denied by insurance
How to fill out prior authorization request form
Who needs prior authorization request form?
A comprehensive guide to prior authorization request forms
Understanding prior authorization
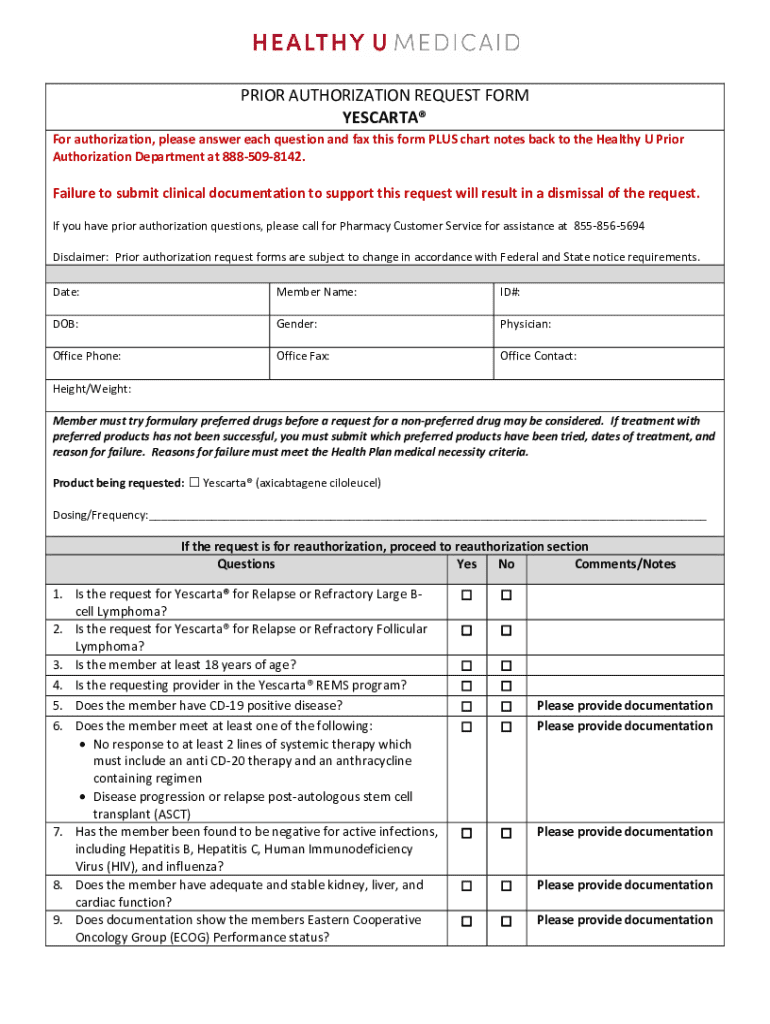
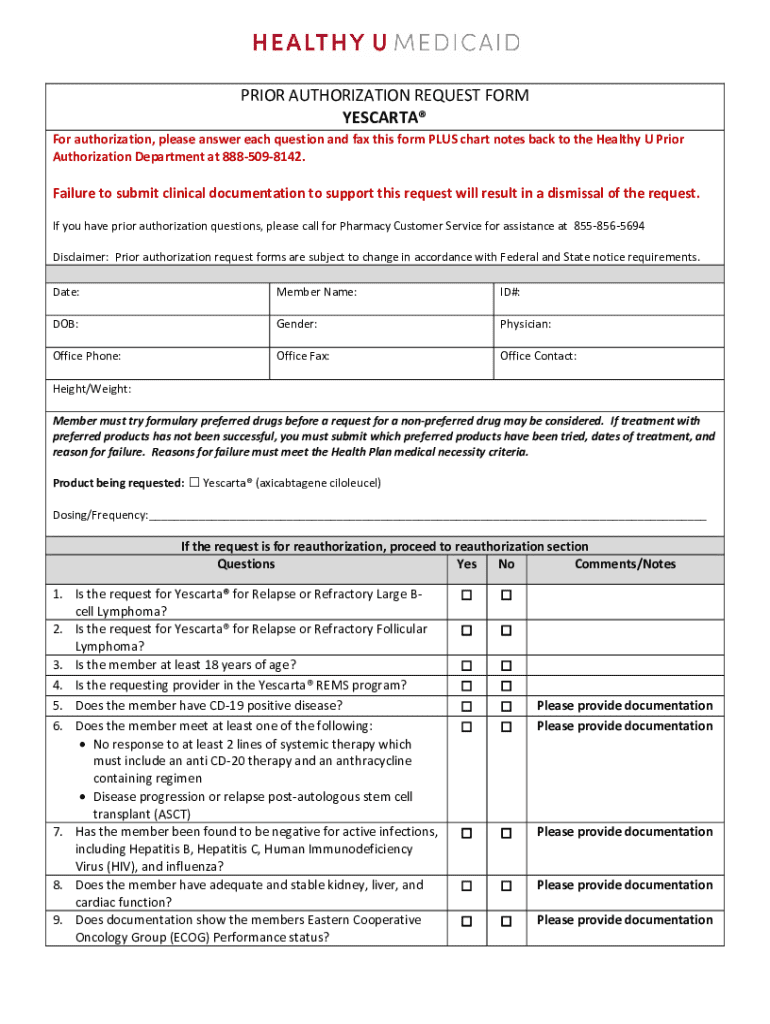
Prior authorization is a cost-control process used by health insurers to determine if a specific service, procedure, or medication is medically necessary before it is delivered to the patient. It involves reviewing requests from healthcare providers to ensure that these actions are justified under the insurance policy terms. The primary purpose of prior authorization is to manage healthcare costs while still ensuring patients receive appropriate care tailored to their medical needs. This process can significantly affect both the patient and provider, as delays in approval can lead to waiting times that may hinder timely access to necessary treatment.
The importance of the prior authorization request form cannot be overstated. Formally, it is a critical document that encapsulates all necessary information needed for insurers to make informed decisions quickly. With accurate and complete submission, providers can streamline their process, ensuring that patients receive timely treatment. The way this form is filled out directly impacts patient care timelines and can be the difference between getting prompt access to medications or treatments and facing unnecessary delays.
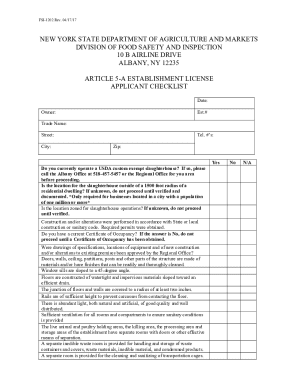
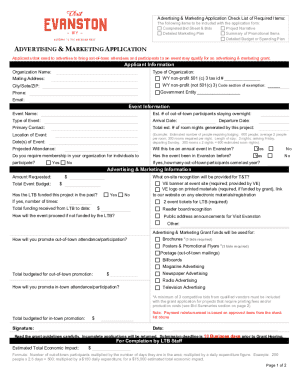
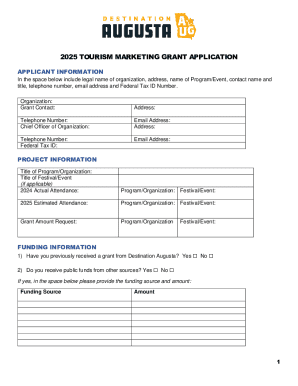
Components of a prior authorization request form
When filling out a prior authorization request form, certain essential information must be included to facilitate prompt processing. Key components include patient identification details such as the patient's name, date of birth, and insurance policy number. Furthermore, provider information specifics are necessary, encompassing provider's name, NPI (National Provider Identifier) number, and contact details. This initial data serves as the foundation for the approval process and identifies the parties involved.
Equally important is documenting medical necessity to substantiate the need for the requested service or medication. This often includes the inclusion of detailed clinical notes, prior treatments tried, and their outcomes. Additionally, it is crucial to ensure that appropriate diagnosis codes, such as ICD-10 codes, correspond to the reason for the authorization request. This comprehensive approach ensures insurers have the information they need to evaluate requests swiftly and fairly.
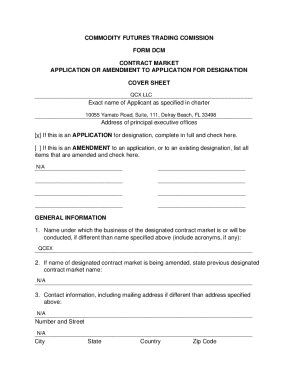
How to access the prior authorization request form
Accessing the prior authorization request form can be done easily through the pdfFiller platform. To locate the form, visit the pdfFiller website and navigate to their library of templates. Users can search for 'prior authorization request form' in the search bar. Once found, the form can be opened in an interactive format, allowing users to start filling it out efficiently.
Alternatively, pdfFiller also offers downloadable versions of the form for those who prefer to work offline. Users can find additional resources and variants of the form directly on the platform, which proves useful for adapting to specific requirements set by different insurance providers. This flexibility ensures users can obtain the necessary documentation quickly, whether online or through traditional methods.
Filling out the prior authorization request form
Filling out a prior authorization request form requires careful attention to detail. Start with Step 1, providing complete patient information, including full name, date of birth, and contact information, as well as the specific insurance details. Step 2 requires you to enter the provider's information, ensuring all data is accurate, including their qualifications and contact methods for any follow-up questions. Providing a direct line for communication can help streamline the process.
Step 3 is where you detail the specific procedure or service requested. This is a crucial component, as the insurer needs to understand clearly what treatment you are seeking. In Step 4, include medical necessity evidence, presenting supporting documentation to validate the request. Common mistakes include failing to complete sections or omitting necessary signatures or dates, which can result in delays or denials. Therefore, double-check all information entered before submission to avoid these pitfalls.
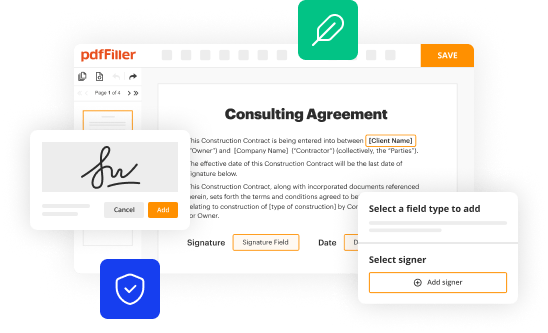
Editing and customizing the form with pdfFiller
One of the standout features of pdfFiller is its editing tools, making it easy to modify pre-existing templates. Users can personalize the prior authorization request form by adding additional notes or comments for clarification, ensuring that every aspect of the request is communicated clearly. With pdfFiller, it becomes straightforward to customize sections on the form, which can help meet specific needs of various insurance companies.
Moreover, the platform's collaborative features allow users to invite team members to review the document. Being able to gather input from multiple stakeholders enhances accuracy, ensuring that nothing important is overlooked. Tracking changes and versions also provides an audit trail, making it easier to navigate edits and ensure the final document reflects the best possible request for prior authorization.
Signing and submitting the form
Once you have filled out and customized the prior authorization request form, the next step is signing it. pdfFiller offers convenient eSignature options, allowing users to sign the document electronically without the need for printing and scanning. This feature not only saves time but also enhances the security and validity of the submission.
After signing, submitting the completed form can be done directly through the pdfFiller platform, streamlining the process even further. Users should be aware of the submission procedures required by their particular insurance provider, which may involve emailing, online submission, or postal mail. Finally, recognizing follow-up protocols is crucial; having a timeline for when to follow up ensures that the request is being processed and avoids unnecessary delays.
Managing submitted authorization requests
Managing the status of submitted authorization requests is vital in ensuring that patients receive timely care. pdfFiller allows users to track their submissions effectively, providing updates on the request's status. This feature reduces anxiety and uncertainty by giving users real-time information on their request's progress.
In cases where additional information is requested by insurers, maintaining effective communication is key. It’s important to respond promptly, clearly outlining any additional documentation needed. If an authorization request is denied, users should be equipped with knowledge about best practices for managing appeals. This includes understanding the reasons for denial and providing the necessary evidence to challenge the insurer's decision.
FAQs on prior authorization
It's common for patients and providers to have questions regarding prior authorization processes. For instance, one frequent query is, 'What should I do if my request is denied?' In such cases, reviewing the denial reasons, correcting any discrepancies, and submitting an appeal are important steps. Another question often asked is, 'How long does the authorization process typically take?' Timeframes can vary greatly depending on the insurer; however, having clear communication and tracking your submission will significantly aid in managing expectations.
Additional resources for getting help with authorization requests include contacting insurer customer service departments or referring to support forums dedicated to healthcare providers. With the right information and guidance, navigating the complexities of prior authorization can be made more manageable.
Benefits of using pdfFiller for prior authorization requests
Utilizing pdfFiller for prior authorization requests offers numerous advantages. The platform allows users to streamline the process from any location, giving them the flexibility to access and manage forms anytime and anywhere. This is particularly beneficial for healthcare providers who are often on the move or managing multiple cases simultaneously.
Collaboration is made easy through pdfFiller, enabling teams to work together in real-time. Features such as live commenting and version tracking improve the document creation process, fostering a team-based approach to managing prior authorizations. Moreover, pdfFiller places emphasis on secure document management, ensuring sensitive patient information remains protected while transferring between parties.
Case studies and success stories
Real-world examples illuminate the effective use of pdfFiller in streamlining the prior authorization request process. Many healthcare providers report reduced processing times and improved patient satisfaction due to the user-friendly capabilities of the PDF platform. By effectively reducing the common hassles noted in traditional methods, successful case studies highlight saved time and less administrative burden on healthcare staff.
Testimonials from teams who have transitioned to pdfFiller reveal positive feedback regarding the efficiency and effectiveness of its tools. Users have expressed how customizable features enhance the documentation process, making the essential task of navigating prior authorization requests less daunting.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit yescarta denied by insurance online?
Can I create an eSignature for the yescarta denied by insurance in Gmail?
How do I fill out yescarta denied by insurance using my mobile device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.