Get the free Prior Authorization Request Form for Prescription Drugs
Get, Create, Make and Sign prior authorization request form



How to edit prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
Your Comprehensive Guide to the Prior Authorization Request Form
Understanding prior authorization
Prior authorization is a critical administrative process required by many health insurance companies before certain medications, procedures, or services are covered. This process aims to ensure that these healthcare services are medically necessary and can help avoid unnecessary costs and complications for both providers and insurers. Without proper authorization, patients may face substantial out-of-pocket expenses.
The role of prior authorization extends beyond cost containment; it actively involves healthcare providers in the decision-making process, ensuring that patients receive the appropriate level of care based on their personal health needs and insurance coverage. This not only facilitates a smoother healthcare experience but also promotes better health outcomes.
Preparing to fill out the prior authorization request form
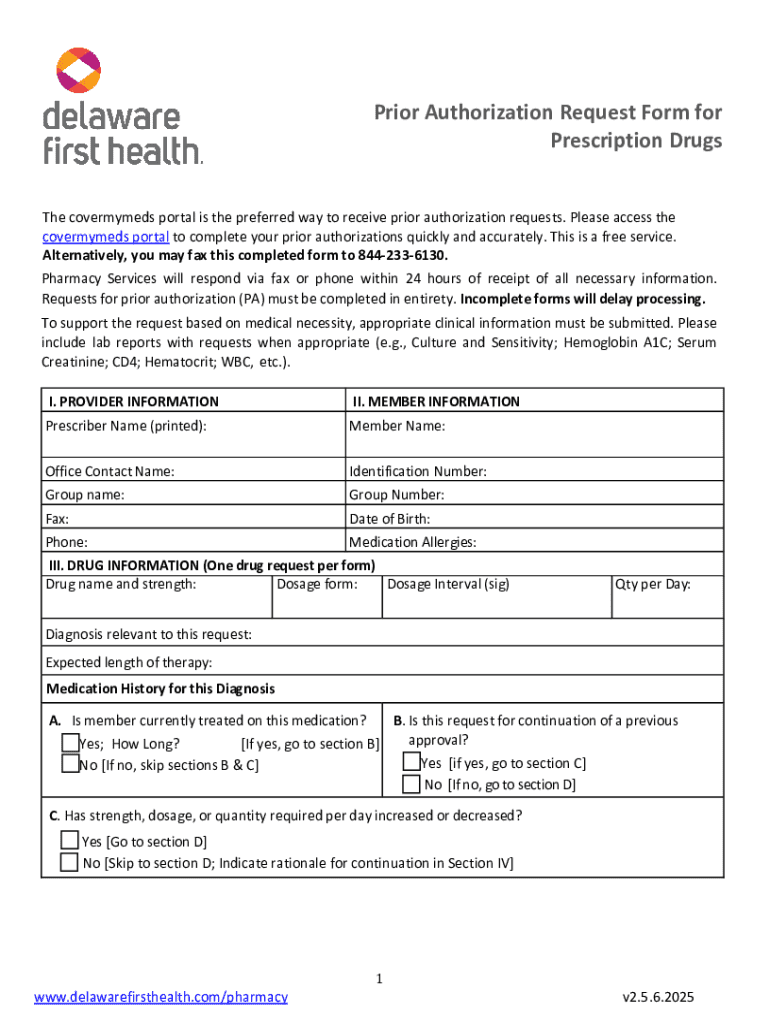
To effectively complete a prior authorization request form, gather all necessary information beforehand. You'll need the patient's details, including their name, date of birth, and insurance specifics, as this information is foundational for any submission. Additionally, the healthcare provider's information such as name, contact details, and NPI (National Provider Identifier) number must be included accurately to avoid complications.
Furthermore, understanding the specific details regarding the requested procedure or medication is crucial. This includes identifying the exact services or medications being requested, their associated codes (like ICD-10 codes), and any medical justification or clinical guidelines that support the necessity of the request.
Step-by-step instructions for completing the prior authorization request form
Accessing the right form is the initial step in a smooth process. Typically, these forms can be found on your insurance provider's website, or through healthcare management platforms like pdfFiller. Ensure that you are using the most recent version of the form, as providers often update their documentation.
Breaking down the sections of the form is essential. The Patient Information Section requires the patient's personal details. Complete accuracy is crucial in the Provider Information Section; double-check that every detail aligns with official records. For the Procedure/Medication Section, it’s not just about naming the medication or procedure—include the corresponding ICD-10 codes and a brief medical justification to support your request. Lastly, gather all supporting documents, which may include clinical notes or test results that substantiate the need for specific treatment.
Reviewing and editing your submission
Ensuring the accuracy of your prior authorization request is imperative, as errors can lead to delays or denials. Before submission, carefully review all sections of the form. Editing plays a crucial role in this process, as it not only enhances clarity but also remedies any potential mistakes that could hinder approval.
Using tools like pdfFiller can assist in the error-checking process. With features designed for collaboration, you can share the request with team members for additional input, ensuring nothing gets overlooked. Such a collaborative approach increases your chances of a successful submission and can save time and resources.
Submitting your prior authorization request
The submission of your prior authorization request can be done through various methods. Many insurance providers offer online portals which streamline the process, while traditional methods such as fax or email are also available. Ensure you are following the specific submission directives provided by the insurer, as each may vary in terms of required documentation or format.
Once submitted, it is essential to track the status of your request. Most insurers will provide a reference number, and contacting the insurer for updates or clarifications can reduce anxiety and improve communication. Keeping a detailed log of your follow-ups is advisable to maintain a clear timeline of the process.
Managing your prior authorization
After submission, it’s critical to understand that response times can vary significantly based on the insurer and the nature of the request. Keeping an eye on notification channels, whether through email or the insurance company’s portal, can help you stay informed. Be patient, but proactive if you haven’t received feedback within the expected timeframe.
In case of a denial, don’t be disheartened. Many requests are declined due to common reasons such as insufficient documentation or failure to meet medical necessity criteria. Familiarizing yourself with these reasons can aid in crafting a robust appeal. Follow up with the insurer to understand specific denial motives, and submit your appeal with supporting documents that comprehensively address these issues.
Utilizing pdfFiller's features for enhanced management
Using pdfFiller can significantly enhance your experience in handling prior authorization requests. The platform allows for easy editing and signing of documents, ensuring that the forms are not only accurate but also legally binding. Interactive document editing can streamline the process, making it relatively painless to adjust or amend prior submissions.
Collaboration is another advantage offered by pdfFiller. With real-time editing and feedback capabilities, you can work effectively with your team to finalize documents quickly. Additionally, cloud-based storage allows you to manage and retrieve documents easily, giving you quick access whenever needed—an essential feature when dealing with time-sensitive requests.
Best practices for future requests
Maintaining accurate records for each prior authorization request helps in streamlining future submissions. Documentation of previous authorizations, including any notes on insurer responses or reasons for denials, serves as an invaluable resource when filling out new forms. This historical knowledge can guide you through current requests effectively.
Furthermore, staying informed on policy changes can significantly affect how you handle these requests. Insurers frequently update their processes and requirements, so subscribing to newsletters or following relevant professional networks can provide updated information on prior authorization regulations and practices.
Testimonials and user experiences
Many users of prior authorization request forms have reported challenges transitioning to the new automated systems. However, numerous case studies highlight successful submissions bolstered by thorough preparation and effective communication with insurers. Individuals and teams that have utilized pdfFiller specifically praise its user-friendly interface and the contribution it has made toward improving efficiency in managing documentation.
Feedback indicates that streamlined document handling has led to better approval rates. Users have noted that clarity in submissions, supported by proper documentation, allows for much smoother transitions through the prior authorization process. These testimonials affirm the value of leveraging digital tools in navigating complex workflows.
Frequently asked questions (FAQs)
Common queries surrounding the prior authorization request process often involve timelines for approval and the types of documentation required. Understanding these nuances can greatly improve your experience. Many users also question how to prepare if a denial occurs and what steps should be taken to appeal effectively.
In terms of pdfFiller-specific queries, users frequently ask about the effectiveness of the editing tools and how collaborative features can be utilized within teams. Addressing these concerns and educating users on available support mechanisms can significantly enhance user satisfaction and reduce frustration during the process.
Contact information and support
When navigating the challenges of prior authorization requests, having access to support can be invaluable. pdfFiller provides dedicated resources to assist users in completing their forms correctly and effectively. Through their community forums, you can connect with others facing similar challenges or share best practices.
Additionally, customer support from pdfFiller is available to address any specific issues or questions. This level of support not only boosts confidence but also contributes to more successful outcomes in prior authorization processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get prior authorization request form?
How do I make changes in prior authorization request form?
How do I edit prior authorization request form on an iOS device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.