
Get the free Wellcare Prior Authorization Form
Get, Create, Make and Sign wellcare prior authorization form
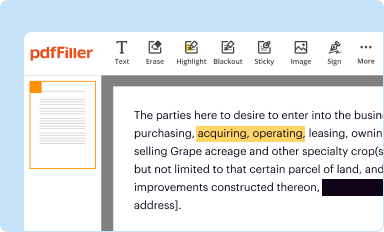
Editing wellcare prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out wellcare prior authorization form
How to fill out wellcare prior authorization form
Who needs wellcare prior authorization form?
Wellcare Prior Authorization Form: A Comprehensive Guide
Understanding the Wellcare prior authorization form
The Wellcare prior authorization form is a crucial tool in the healthcare system, designed to manage the approval process for specific medical services and medications. Prior authorization is essentially a process that healthcare providers must follow to gain approval from Wellcare before proceeding with certain treatments or medications for their patients. The purpose of this process is to ensure that the requested service is medically necessary, cost-effective, and within the plan's coverage guidelines. For patients, this translates to a streamlined pathway to receive necessary medical care while ensuring that the costs are justified and covered by their health plan.
The Wellcare prior authorization form aids in finalizing this process, making it essential for healthcare providers and patients alike. Its importance cannot be overstated, as completing the form accurately can greatly affect treatment timelines and patient satisfaction. A well-submitted prior authorization form helps facilitate prompt decisions that can directly impact patient care.
When is a prior authorization required?
Prior authorizations are typically required in specific situations to prevent unnecessary expenses and ensure the appropriateness of care. Services that often necessitate prior authorization include high-cost medications, elective surgeries, and advanced imaging studies such as MRI and CT scans. For example, if a patient requires a new medication that is not on the formulary or a specialized treatment plan, a prior authorization will be necessary.
In the case of Wellcare, they play an essential role in determining whether a request for these services is valid under their guidelines. Each Wellcare plan may have different requirements regarding what needs authorization, and providers must check Wellcare's specific criteria to ascertain if prior authorization applies to their patient’s needs.
Getting started with the Wellcare prior authorization form
For those looking to initiate the prior authorization process, the first step is obtaining the Wellcare prior authorization form. This form is readily available on the Wellcare website or can be accessed through the healthcare provider's office. Additionally, pdfFiller offers a downloadable PDF version of the form, ensuring users can easily access and fill it out from anywhere. This accessibility is crucial for busy healthcare providers and teams managing multiple authorizations.
In some cases, Wellcare may have different versions of their prior authorization forms, depending on the type of service requested. It’s vital to ensure that the correct version is utilized, as using an incorrect form can lead to unnecessary delays in the authorization process. Understanding which form applies to specific situations can save time and improve the chances of a swift approval.
Detailed instructions for filling out the Wellcare prior authorization form
Filling out the Wellcare prior authorization form correctly is crucial for a successful submission. Start with the patient information requirements, which typically include the patient's name, date of birth, and insurance details. This section establishes the eligibility of the patient under Wellcare’s plans and helps to speed up the review process.
Next, provide detailed provider information, including the healthcare provider's name, contact details, and NPI number. Following that, specify the service or medication in question. Clearly articulate the clinical justification supporting the request. Adequate documentation is key, often involving attaching relevant clinical notes or lab results that substantiate the need for the service.
Submitting the Wellcare prior authorization form
Once the Wellcare prior authorization form is completed, it's time to submit it using one of the accepted methods. Wellcare typically accepts submissions via their online portal, where providers can upload the form securely. This method is advantageous as it allows for immediate transmission and easier tracking of the submission status.
Alternatively, providers have the option to mail or fax the completed form. Regardless of the submission method, it’s crucial to adhere to submission deadlines and be cognizant of the timeframes outlined by Wellcare. Being proactive about these deadlines helps avoid disruptions in care for patients.
What happens after you submit the form?
Following the submission of the Wellcare prior authorization form, it enters a review process conducted by Wellcare’s clinical staff. This team evaluates the information provided and decides whether the requested service meets the medical necessity criteria set forth by the insurance plan. In general, the review process can take several business days; however, urgent requests may be expedited.
Providers are typically able to track the status of their submissions through the online portal, gaining insights into whether the request is still under review or if a decision has been made. This transparency can enhance communication between providers and patients, allowing for better anticipation of when treatment can commence.
Understanding authorization determinations
Once Wellcare has completed its review of the prior authorization request, the healthcare provider will receive one of three possible outcomes: approval, denial, or a request for additional information. An approval indicates that the service is covered, and the provider can proceed with the treatment plan as requested.
If denied, the provider will need to reassess the request and consider providing additional documentation or justification as needed. Likewise, if additional information is requested, prompt provision of the required details is essential to prevent further delays in treatment. Understanding these outcomes helps providers manage patient expectations effectively.
Managing prior authorizations with Wellcare
Handling prior authorizations efficiently is crucial in healthcare. If a provider needs to amend or withdraw a prior authorization request after submission, they can typically do so by contacting Wellcare directly. This flexibility ensures that providers can adapt to changing patient needs or correct any submission errors.
Additionally, in the event of a denial, providers can initiate a dispute or reconsideration process. Wellcare provides resources to assist with these requests, ensuring that providers have access to necessary information for successful appeals. Utilizing these resources can significantly alleviate administrative burdens and support patient care.
Interactive tools and resources for better management
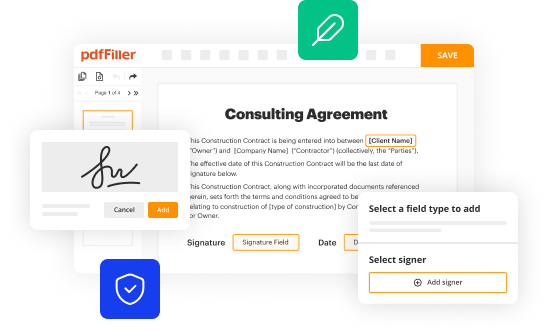
In today’s digital age, leveraging online resources can greatly enhance the experience of managing prior authorizations. pdfFiller's platform is particularly beneficial as it offers a suite of interactive tools designed to streamline the documentation process. Users can create, edit, and eSign their Wellcare prior authorization forms easily without navigating through cumbersome paper trails.
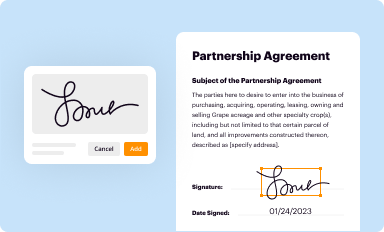
Collaborative features allow teams to work together on documents in real-time, ensuring that all necessary information is compiled efficiently. The ability to use eSigning capabilities on the pdfFiller platform fast-tracks approvals, allowing documents to be signed and submitted without the traditional delays associated with printing and mailing.
Key considerations for providers and patients
For healthcare providers and patients alike, there are several best practices to follow when dealing with the Wellcare prior authorization form. Ensuring that the form is completed accurately and thoroughly the first time can significantly reduce the chances of delays or denials. Providers should familiarize themselves with Wellcare’s policy guidelines, ensuring that requests align with coverage criteria.
Moreover, it’s essential to communicate regularly with patients about the status of their authorization requests. This proactive approach keeps patients informed and helps to manage their expectations throughout the process. Support channels, such as customer service at Wellcare or resources from pdfFiller, can provide valuable assistance if challenges arise.
Real-life scenarios and case studies
Examining real-life scenarios can shed light on the practical implications of the Wellcare prior authorization form. For instance, a healthcare provider may submit a request for a brand-name medication that is vital for managing a patient’s chronic condition. If the request is well-documented and clearly justifies the medical necessity, it is more likely to result in an approval.
Conversely, a request that lacks sufficient documentation or does not meet the medical necessity criteria may lead to a denial. Such cases emphasize the need for comprehensive and accurate submissions, showing how effective use of the Wellcare prior authorization form can significantly impact patient outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the wellcare prior authorization form electronically in Chrome?
How do I complete wellcare prior authorization form on an iOS device?
How do I complete wellcare prior authorization form on an Android device?
What is wellcare prior authorization form?
Who is required to file wellcare prior authorization form?
How to fill out wellcare prior authorization form?
What is the purpose of wellcare prior authorization form?
What information must be reported on wellcare prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.















