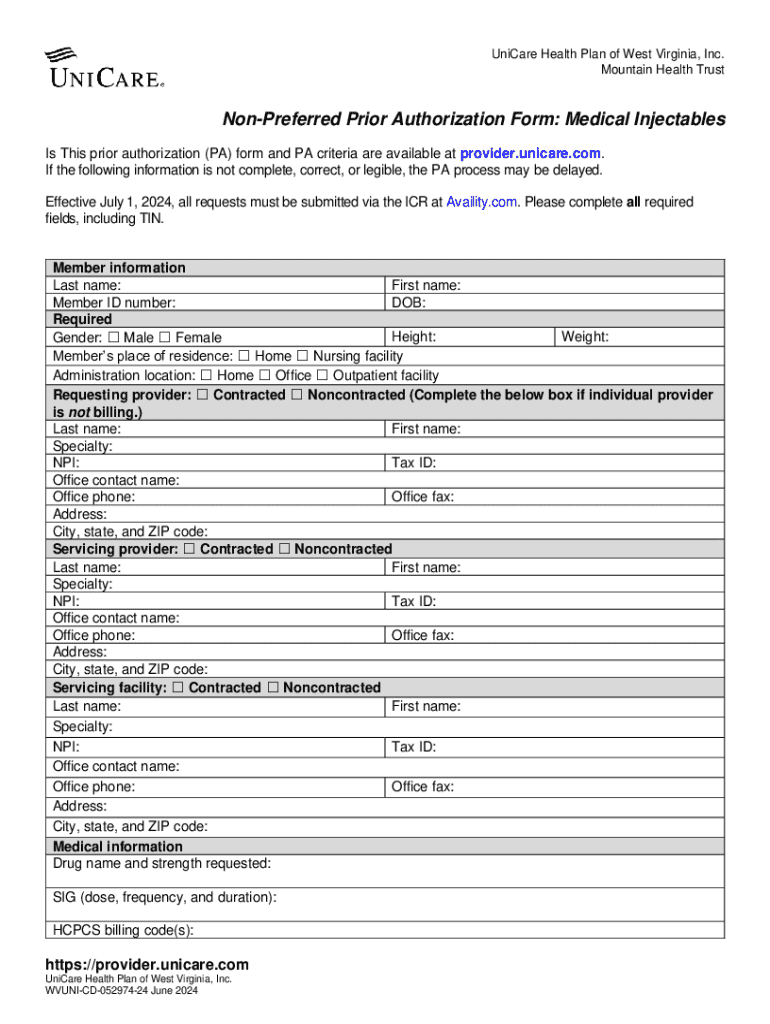
Get the free Non-preferred Prior Authorization Form: Medical Injectables
Get, Create, Make and Sign non-preferred prior authorization form



How to edit non-preferred prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out non-preferred prior authorization form

How to fill out non-preferred prior authorization form
Who needs non-preferred prior authorization form?
Understanding Non-preferred Prior Authorization Forms
Understanding non-preferred prior authorization forms
A non-preferred prior authorization form is a specific document required by healthcare insurance providers when a provider seeks approval for a treatment or medication that is not on the insurance plan's preferred drug list. The purpose of this form is twofold: it ensures that patients receive necessary medical treatments while also controlling costs for insurers. By requiring healthcare providers to submit this form, insurance companies can evaluate whether a treatment is medically necessary and appropriate for the patient.
These forms play a critical role in healthcare settings as they help facilitate communication between healthcare providers and insurance companies, ultimately aiming to promote patient safety and quality of care. Non-preferred prior authorization forms are particularly relevant in ensuring that patients receive treatments that may not be readily accessible under standard insurance guidelines.
Differences between preferred and non-preferred forms
One of the key distinctions between preferred and non-preferred prior authorization forms lies in their designations by insurance companies. Preferred medications and treatments are typically those that insurers cover in full or at a minimal copayment, encouraging both compliance and patient satisfaction. Conversely, non-preferred options may require more extensive documentation and justification to gain approval, often leading to delays in patient care.
The impact of these differences can profoundly affect patient care, treatment satisfaction, and overall outcomes. Delays due to prior authorization, especially for non-preferred requests, can lead to worsening health conditions and extended recovery times.
Identifying when a non-preferred prior authorization is required
Understanding the situations that might trigger a non-preferred prior authorization form can help healthcare providers proactively address insurance requirements. Common medical conditions like chronic pain management, specialty medications for conditions like multiple sclerosis or rheumatoid arthritis, and specific surgical procedures often necessitate the non-preferred authorization route.
Additionally, certain insurance policies have specific exclusions, requiring prior authorization even for more routine or commonly prescribed treatments. Knowledge of these exclusions is vital for seamless patient care and treatment continuity.
How to verify insurance requirements
To effectively manage non-preferred authorizations, verifying insurance requirements is crucial. Begin by directly contacting the insurance provider or using their online member services portal to clarify what treatments need authorization. This information can often be located in the insurance policy documents or provider manuals, which might also detail necessary clinical criteria.
Documentation and reference guides offered by insurers can assist in understanding authorization requests, and are beneficial in avoiding unnecessary delays. Many insurance companies have dedicated customer service lines for inquiries regarding coverage and prior authorization protocols against defined treatment options.
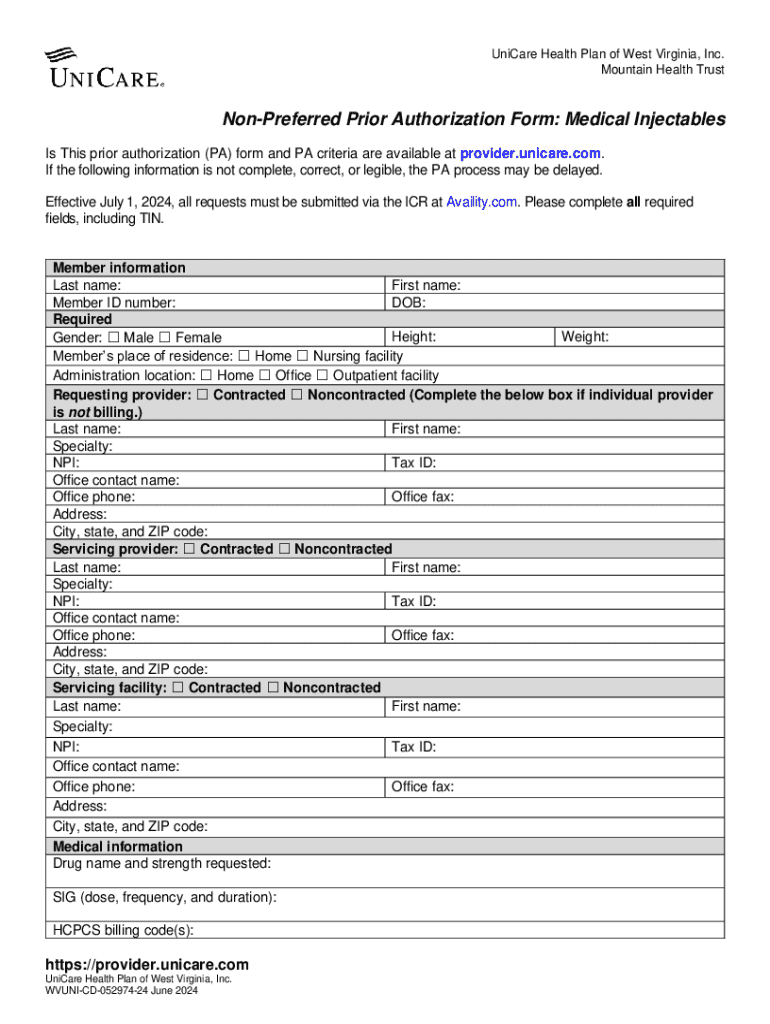
Step-by-step guide to completing a non-preferred prior authorization form
Filling out a non-preferred prior authorization form correctly is paramount to avoid delays in care. Begin by gathering all required information, including patient demographics, insurance information, and both prescribing and performing provider details. Additionally, having necessary clinical records and lab results will substantiate the need for the prescribed treatment.
Each section of the non-preferred prior authorization form requires attention to detail. Ensure that you fill out the patient's medical history accurately and state the reasons for recommending non-preferred treatments clearly. Common mistakes to avoid include incomplete fields, missing signatures, and incorrect patient information, which can delay the review process.
Submitting the form
Submission methods for non-preferred prior authorization forms vary by insurance provider. Familiarize yourself with the submission process, whether it be through online portals, facsimiles, or in-person delivery. Follow up consistently to ensure timely processing, noting any reference numbers given upon submission to track the request.
Understanding the review timeline is equally essential. Typically, most insurance providers offer a review period ranging from 48 hours to several weeks, depending on the complexity of the request. Document any follow-up communications to ensure proper tracking.
Tools and resources for managing non-preferred prior authorization forms
Utilizing digital document management tools, such as pdfFiller, can significantly enhance the efficiency of filling out and submitting non-preferred prior authorization forms. pdfFiller provides various editing and collaboration features, allowing healthcare teams to fill out forms quickly and efficiently. The platform supports electronic signatures, providing a seamless method for obtaining necessary sign-offs from providers.
Moreover, pdfFiller offers a repository for storing completed forms, which is essential for reference during future authorizations and tracking. Users have access to examples of non-preferred prior authorization forms relevant to a range of scenarios, ensuring that they have the correct templates readily available for use.
Handling potential challenges and denials
Despite best efforts, non-preferred prior authorization requests can be denied for several reasons. Common causes include insufficient clinical rationale, a lack of essential documentation, or not following payer-specific requirements. Understanding these policies can improve successful outcomes in the authorization process.
When a denial occurs, preparation for an appeal is crucial. Start by carefully reviewing the denial reasons and gathering documentation that supports the treatment necessity. This may involve compiling medical records, lab results, and previous treatment information to substantiate your case. Establish effective communication with insurance representatives to clarify denial reasons and discuss next steps.
Best practices for future non-preferred form submissions
Staying updated on policy changes related to non-preferred prior authorization forms is essential in maintaining smooth health care delivery. Policies shift as insurance regulations evolve, impacting approval processes. Regular communication with insurance providers can alleviate confusion regarding recent changes and enhance your approach toward filling out necessary forms.
Building a repository of submitted forms allows for streamlined future authorization requests. Keeping organized records of past submissions enables quick reference that not only assists in repetitive authorizations but also builds a case history for ongoing patient care.
Engaging with the community
Experience sharing among healthcare professionals when dealing with non-preferred prior authorization forms can lead to fortified relationships and enriched practices. Use community forums or social media groups to discuss tips, strategies, and common challenges faced during the form submission process.
Keeping connected with healthcare professionals helps to remain updated on best practices and policy shifts that impact non-preferred filings. Engaging in these networks can strengthen collaborative efforts and improve patient outcomes across the board.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find non-preferred prior authorization form?
How can I edit non-preferred prior authorization form on a smartphone?
How do I edit non-preferred prior authorization form on an iOS device?
What is non-preferred prior authorization form?
Who is required to file non-preferred prior authorization form?
How to fill out non-preferred prior authorization form?
What is the purpose of non-preferred prior authorization form?
What information must be reported on non-preferred prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.