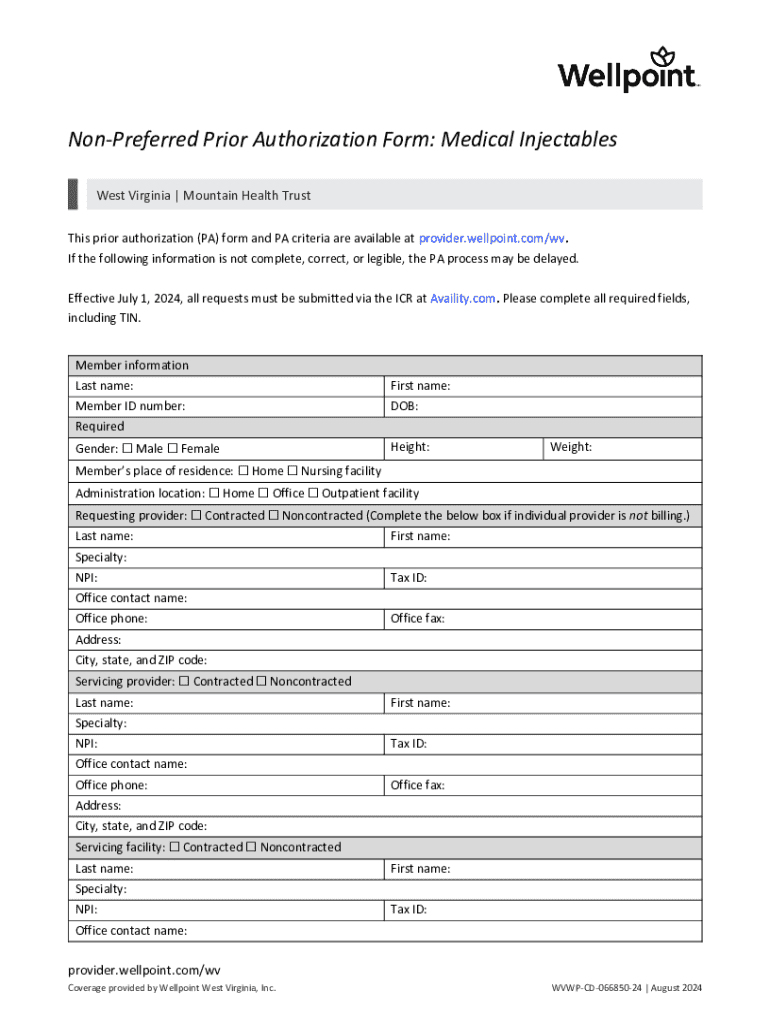
Get the free Non-preferred Prior Authorization Form: Medical Injectables
Get, Create, Make and Sign non-preferred prior authorization form



Editing non-preferred prior authorization form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out non-preferred prior authorization form

How to fill out non-preferred prior authorization form
Who needs non-preferred prior authorization form?
Navigating the Non-Preferred Prior Authorization Form: A Comprehensive Guide
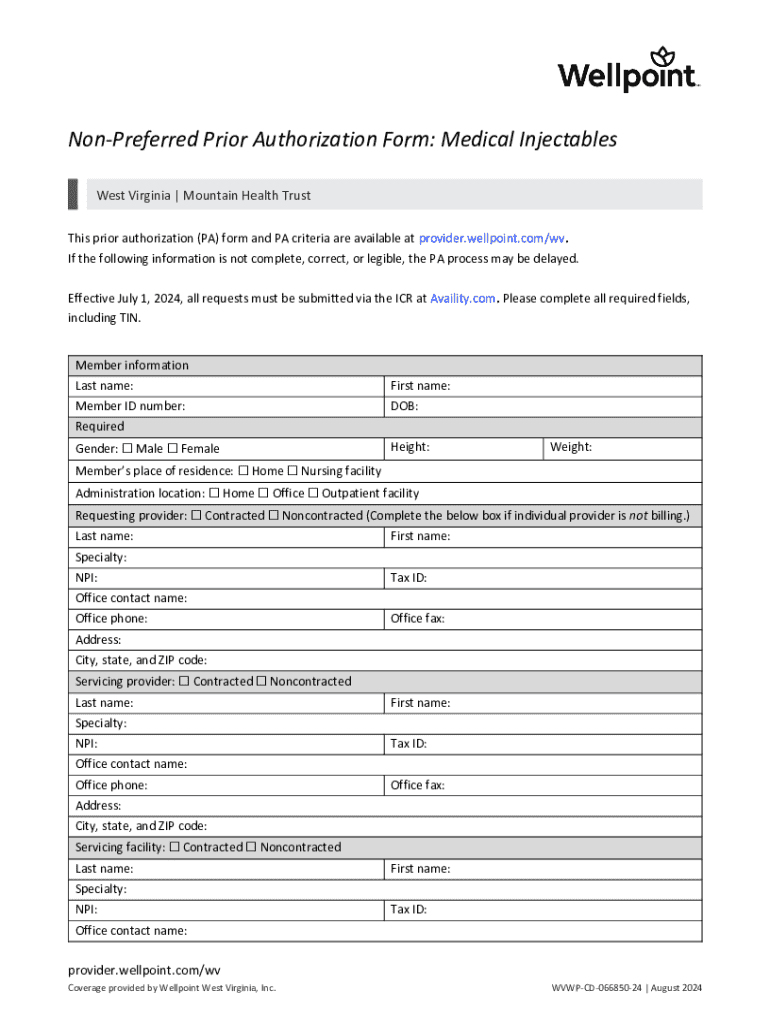
Understanding non-preferred prior authorization forms
A non-preferred prior authorization form is a crucial document used in the healthcare system to obtain approval for treatments or medications that are not listed as preferred by a patient's insurance provider. This authorization is essential as it ensures that the chosen treatment aligns with the insurance provider’s coverage policies. Without this approval, healthcare providers may struggle to secure reimbursement for non-preferred services, impacting the financial aspects of patient care.
Understanding the role of non-preferred prior authorization is vital for healthcare professionals, as it ensures that necessary treatments can be delivered in a timely fashion without financial burdens. Unlike preferred services where approvals may be more streamlined, non-preferred authorizations require a comprehensive justification to establish medical necessity and obedience to the insurance plan's guidelines.
Common use cases for non-preferred prior authorization
Non-preferred prior authorization forms are commonly required in various scenarios such as specific treatments, high-cost medications, or specialized services that might not be listed under a provider's existing insurance plan. For example, a patient requiring an expensive brand-name medication for a chronic illness may need this prior approval if a generic version is preferred by the insurance company. The healthcare provider must submit the non-preferred prior authorization to obtain necessary approval for the prescribed treatment.
Key stakeholders in this process encompass the patient, healthcare provider, and insurance company. Each plays a pivotal role in determining the approval of the requested treatment. The delay or denial of a non-preferred prior authorization can significantly affect patient care and treatment plans, potentially leading to interruptions in therapy or non-compliance due to cost. Therefore, prompt and effective management of these forms is essential.
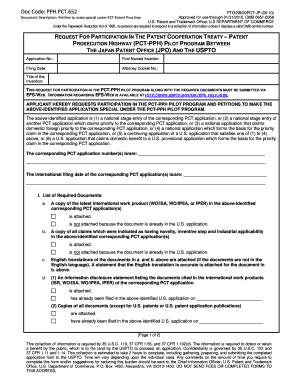
Preparing to complete the non-preferred prior authorization form
Before filling out a non-preferred prior authorization form, it is crucial to gather all necessary information to ensure the submission is complete and accurate. Start with the patient's details including full name, date of birth, and insurance policy number. Next, provide relevant provider details such as the physician's name, contact information, and their National Provider Identifier (NPI) number. It is essential also to collect the specific medical information that pertains to the patient's condition and the requested treatment or medication.
Understanding the requisite documentation that supports the authorization request, such as previous treatment records and test results, is critical. These documents will validate the need for the non-preferred treatment prescribed and strengthen the claim for approval. Additionally, prior to submission, verifying the patient's eligibility and insurance coverage is a crucial step. This assures that the treatment under discussion is covered, minimizing potential complications in the process.
Step-by-step guide to filling out the non-preferred prior authorization form
Filling out a non-preferred prior authorization form can seem daunting, but breaking it down into manageable sections can help streamline the process. The first section typically requires patient information. It's essential to accurately fill in details such as full name, date of birth, and insurance policy number. However, ensure you double-check for common mistakes such as typos, which can delay the authorization process.
The second section focuses on provider information. It’s important to accurately represent the provider's network status. Make sure to input correct details about the provider's practice and National Provider Identifier (NPI) number. This will facilitate faster processing. The third section deals with treatment information, where you should specify drug names or services. Not only do you need to be precise here, but it’s also useful to mention any timeframes or urgency regarding the treatment to emphasize the necessity.
The fourth section is dedicated to the medical necessity justification. This part requires a solid articulation of why the requested treatment is deemed necessary, particularly due to the non-preferred status. Supporting this section with relevant clinical data or studies can significantly boost your chances of approval. Lastly, the fifth section covers signatures and authorization — obtaining the necessary signatures from the provider and potentially the patient is paramount. Electronic signature options, such as those provided by pdfFiller, can simplify this process.
Tips for effective submission of non-preferred prior authorization
Submitting a non-preferred prior authorization form correctly is crucial for successful approval. Recommended methods for submission include utilizing online platforms offered by insurance companies, as these often offer instant receipt confirmation and can expedite processing. If submitting via fax or postal service, always ensure that you maintain copies of the sent documents and follow up if you do not receive confirmation within a reasonable time frame.
Additionally, it's wise to create a checklist prior to submission that includes double-checking all filled out sections, securing needed documentation, and confirming the delivery method used. Confirming receipt of authorization requests, whether online or manual, is essential for peace of mind and tracking progress in the authorization process.
Tracking the status of your non-preferred prior authorization request
Once your non-preferred prior authorization request has been submitted, understanding how to track its status is invaluable for both the provider and the patient. Many insurance companies offer online portals where the status can be easily checked. It’s beneficial to familiarize yourself with these tools, which often provide the current progress of the request.
Understanding the typical timelines to expect can aid in managing patient expectations, ensuring they are informed of any delays or necessary follow-ups. In cases where authorization is denied, it is vital to know the appeals process. Generally, this involves submitting additional information that supports the medical necessity of the treatment or medication. Consulting resources such as the insurance provider’s handbook or customer service can provide direction on how best to proceed.
Utilizing pdfFiller for enhanced document management
pdfFiller is an exceptional tool for streamlining the non-preferred prior authorization form process. With its seamless editing capabilities, users can easily modify fields and input accurate information. The eSigning solutions offered allow for timely approvals, especially crucial in scenarios where quick authorization is necessary. Collaboration tools enable teams to work together on documents, ensuring accuracy and compliance are met efficiently.
Moreover, pdfFiller's cloud-based storage ensures that your forms and documents are securely managed, making retrieval simple and hassle-free whenever needed. Integration with other healthcare platforms further enhances the versatility of pdfFiller, providing an all-in-one solution for document management, catering specifically to the needs of healthcare providers navigating the complexities of non-preferred prior authorizations.
Real-world examples and case studies
Successful management of non-preferred prior authorizations can lead to significant improvements in patient care. For instance, consider a case where a physician effectively utilized a non-preferred prior authorization form for a patient with epilepsy. By providing thorough documentation and supporting clinical studies, the physician not only secured approval for a unique medication but also facilitated timely treatment that significantly enhanced the patient's quality of life. Such success stories are increasingly common as healthcare providers become adept at navigating this often complex process.
Conversely, there are lessons to be learned from common pitfalls. For instance, inadequate communication between the provider and patient can lead to misunderstandings and delays. Properly managing expectations and ensuring that the patient is informed about the steps involved in the prior authorization process are essential to prevent this. It highlights the need for vigilance and attention to detail in submissions, as this can ultimately affect treatment outcomes.
FAQs about non-preferred prior authorization
Addressing common queries surrounding non-preferred prior authorization forms can clarify misconceptions and ease anxiety for healthcare professionals and patients alike. A frequent question concerns the timeline for obtaining approval. While it can vary, insurance companies generally communicate their decision within a few days to a couple of weeks, depending on the level of detail required in the submission. Perceptions also exist regarding the difficulty of getting approvals for non-preferred medications; understanding the detailed justifications needed can equip providers with the necessary tools for success.
Additionally, another common concern is the impact on patient care. Providers often wonder if the lengthy process of obtaining prior authorization may delay necessary treatments. To alleviate this, prompt completion and submission of forms along with proactive follow-ups can significantly mitigate potential delays, ensuring that patients receive prompt and necessary care, regardless of the authorization status.
Conclusion: Mastering the non-preferred prior authorization process
Mastering the non-preferred prior authorization process is crucial for healthcare providers who strive to deliver high-quality, uninterrupted patient care. Understanding the intricacies involved—from preparation to tracking the authorization status—saves time and reduces frustration both for providers and patients. By effectively utilizing tools like pdfFiller, which streamlines the process through seamless document management, providers can navigate these complexities with greater ease.
Ultimately, familiarity with the non-preferred prior authorization forms enables healthcare practitioners to advocate successfully for their patients. Empowered by knowledge and streamlined technologies, such as pdfFiller, users can enhance their documentation practices and ensure patients receive the necessary care without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get non-preferred prior authorization form?
How do I edit non-preferred prior authorization form on an iOS device?
How do I complete non-preferred prior authorization form on an iOS device?
What is non-preferred prior authorization form?
Who is required to file non-preferred prior authorization form?
How to fill out non-preferred prior authorization form?
What is the purpose of non-preferred prior authorization form?
What information must be reported on non-preferred prior authorization form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.