Get the free Cobra Coverage Election Form
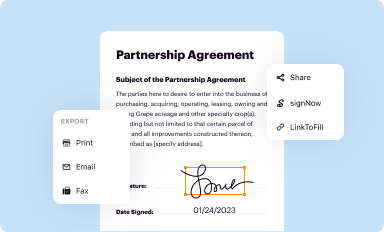
Get, Create, Make and Sign cobra coverage election form
How to edit cobra coverage election form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cobra coverage election form
How to fill out cobra coverage election form
Who needs cobra coverage election form?
Cobra Coverage Election Form: A Comprehensive How-to Guide
Understanding COBRA Coverage
COBRA (Consolidated Omnibus Budget Reconciliation Act) coverage allows individuals to maintain their employer-sponsored health insurance after experiencing job loss, reduced work hours, or other qualifying events. Understanding COBRA is crucial for securing continuous health care during uncertain times.
The importance of COBRA coverage cannot be overstated; it acts as a safety net, offering necessary health benefits when individuals or their families experience employment transitions. COBRA ensures that gaps in coverage are minimized, protecting individuals from the potential financial burdens associated with losing health insurance.
Key benefits of COBRA coverage
COBRA coverage offers multiple advantages that can significantly support individuals during an already challenging time. Its primary feature is the continuity of health coverage, ensuring that you don’t lose access to your benefits, including preventive services and medications that you have been utilizing.
One major benefit is coverage for dependents. If you were the primary policyholder, your dependents can also continue receiving coverage under your plan, thereby maintaining family health security. Preventing gaps in insurance prevents individuals from discovering unexpected medical costs that arise from a lack of coverage.
The COBRA election process
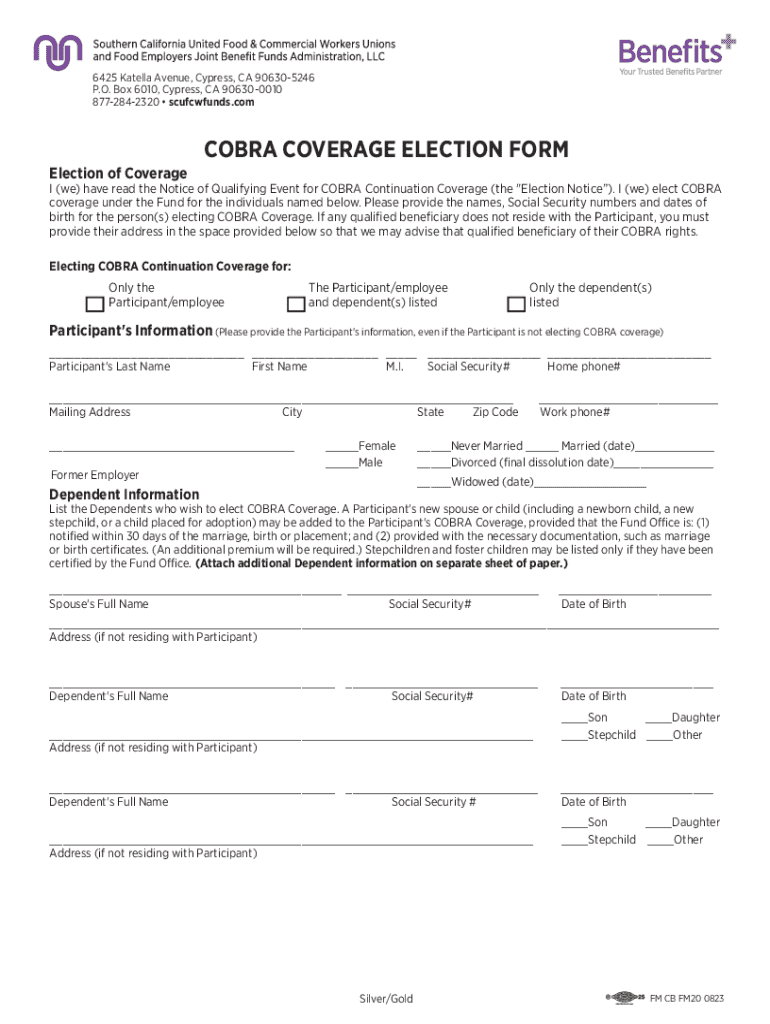
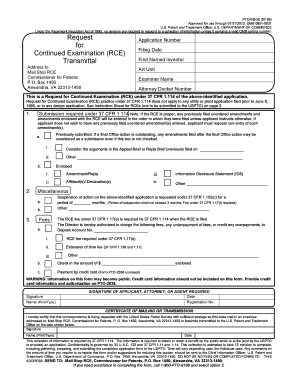
Initiating COBRA coverage requires understanding the election process, starting with the COBRA Election Form. This form is your official request to continue your health insurance benefits, allowing you to exercise your rights under COBRA.
What is the COBRA election form?
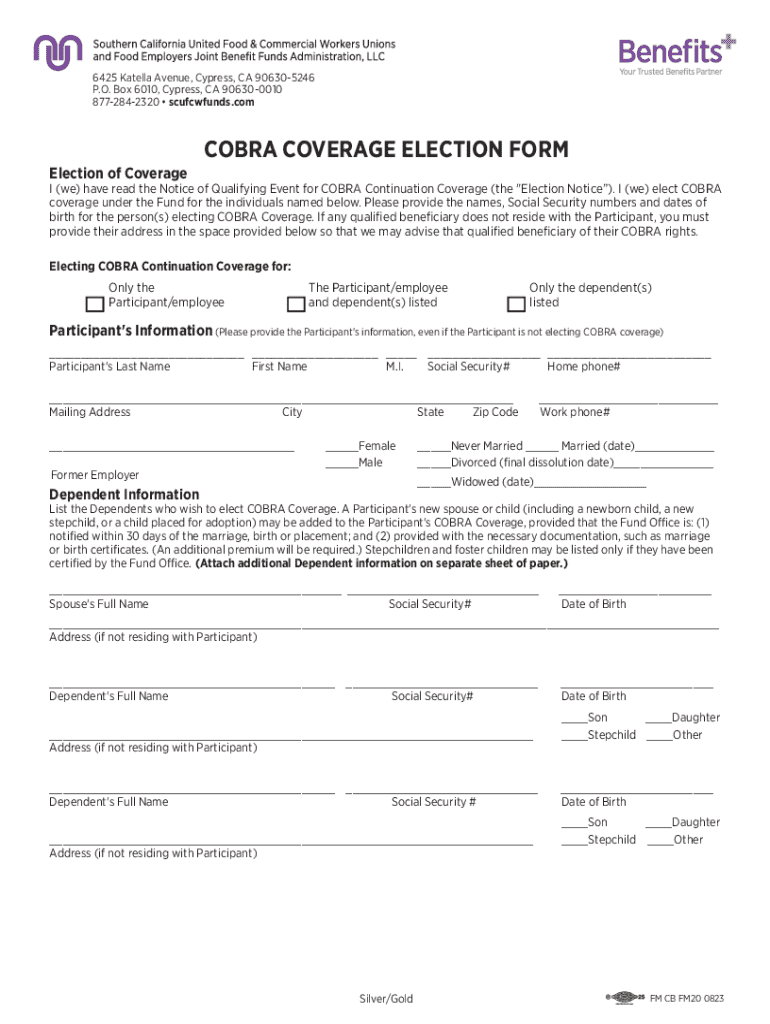
The COBRA Election Form serves as an essential document in the election process. It captures crucial details that validate your request to elect health coverage continuation. This form typically includes personal information, the type of coverage you wish to elect, and any dependent coverage preferences.
Obtaining your COBRA election form
Employers are responsible for sending the COBRA election form to former employees or covered dependents following a qualifying event. Depending on the employer, this could take place within 14 days post-qualifying event. It's important to monitor your mail carefully to ensure you don’t miss this important document.
Completing the COBRA election form
Filling out the COBRA election form accurately is crucial. Begin by reviewing all the information requested on the form—this typically includes your name, address, dates, and the specific type of coverage you are electing. Ensure that all your information is current and correctly reflects your situation.
Submitting your COBRA election form
After filling out the COBRA election form, it’s essential to submit it promptly. Send your completed form to the specified department within your employer's organization, adhering to the deadlines outlined in your election notice. Missing the deadline could forfeit your right to COBRA coverage.
Understanding your rights and responsibilities with COBRA
Being aware of your rights under COBRA is vital. Upon electing coverage, you should receive essential notices regarding your health insurance, premium costs, and any changes. Furthermore, you hold the right to maintain your coverage for a set period, typically 18 months, and you must comply with premium payment requirements to keep your coverage active.
If you miss the COBRA election window, your right to continue coverage can lapse, leaving you vulnerable without health insurance. Additionally, your employer has specific obligations regarding notifying you about your rights and coverage options, ensuring that you are well-informed.
FAQs about COBRA and the election process
Common concerns regarding the COBRA election process are normal, especially in times of transition. If you haven't received a COBRA election letter, it's advisable to contact your employer's HR or benefits department immediately to ensure you haven't missed your opportunity.
Upon submitting the form, changes may not be possible, as the elections you make are usually final. Should your employer fail to comply with COBRA regulations, there are procedures you can pursue, including filing a complaint with the Department of Labor.
Managing your COBRA coverage
Once you elect to continue your COBRA coverage, effective management can make your experience smoother. Keep your documents organized and stay on top of deadlines for premium payments. A dedicated folder—physical or digital—can help track your health benefits, payment records, and correspondence.
Regular communication with your employer's benefits department is also essential. Should there be changes in your situation or questions about your coverage, proactive outreach to clarify terms can prevent issues down the line. Furthermore, maintaining a regular check on your payment status will help ensure you never inadvertently lapse in your coverage.
Additional considerations
Transitioning off COBRA can raise questions about what to expect. Typically, you'll be presented with options to enroll in a new health plan during this transition, whether that involves moving to an individual policy or qualifying for a new employer’s insurance.
Exploring other alternatives for health coverage may be beneficial, especially if you no longer qualify for COBRA. State or federal exchange programs, Medicaid, or private insurance plans can fill in the gaps. It’s advisable to research diligently to understand your options before your COBRA coverage concludes.
Getting help and support for COBRA questions
Navigating COBRA can be intricate, and having a support system or reliable resources can alleviate anxiety. Contacting your employer's benefits department is often the first step to clarifying any questions or issues regarding your COBRA election form and coverage.
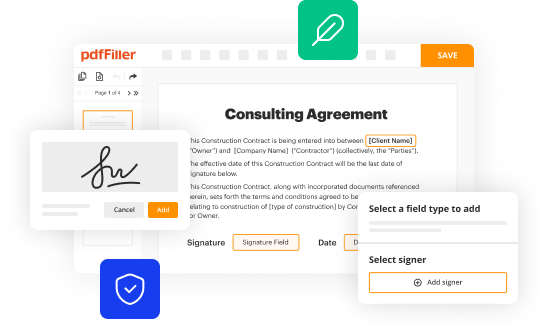
Consumer advocacy groups can also provide insight and support regarding your rights under COBRA. Additionally, for those looking to simplify the interaction with COBRA documents, pdfFiller offers an innovative solution to edit, eSign, and manage COBRA forms easily.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify cobra coverage election form without leaving Google Drive?
How can I send cobra coverage election form for eSignature?
How can I edit cobra coverage election form on a smartphone?
What is cobra coverage election form?
Who is required to file cobra coverage election form?
How to fill out cobra coverage election form?
What is the purpose of cobra coverage election form?
What information must be reported on cobra coverage election form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.