Get the free Prior Authorization Request
Get, Create, Make and Sign prior authorization request



How to edit prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request

How to fill out prior authorization request
Who needs prior authorization request?
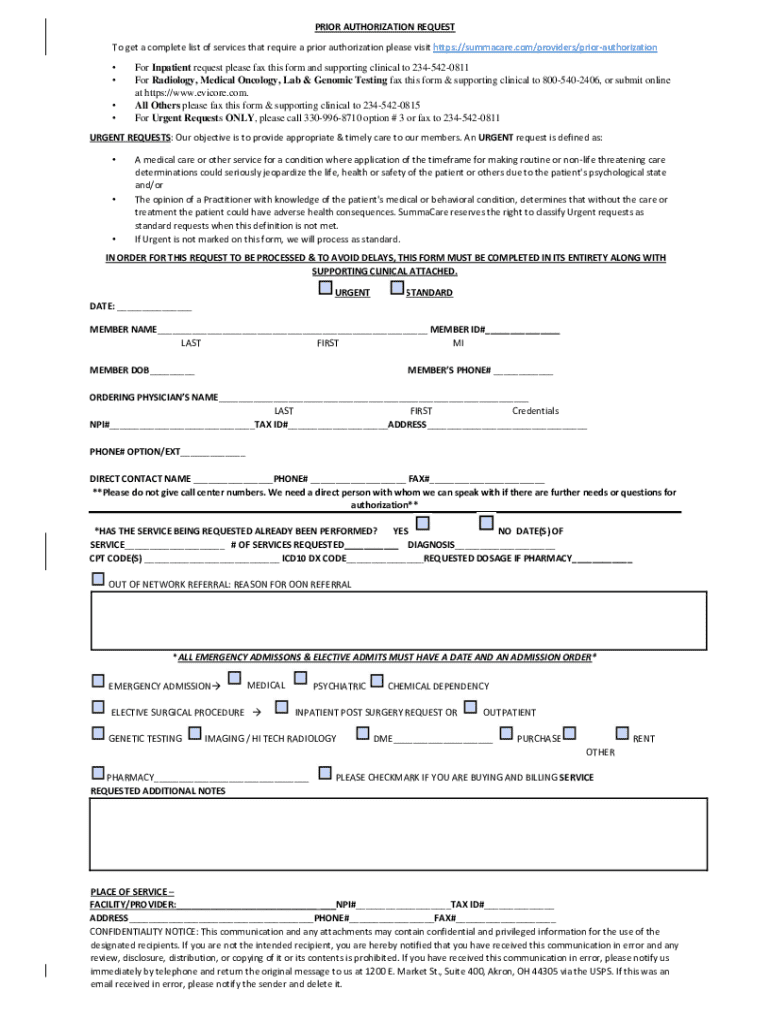
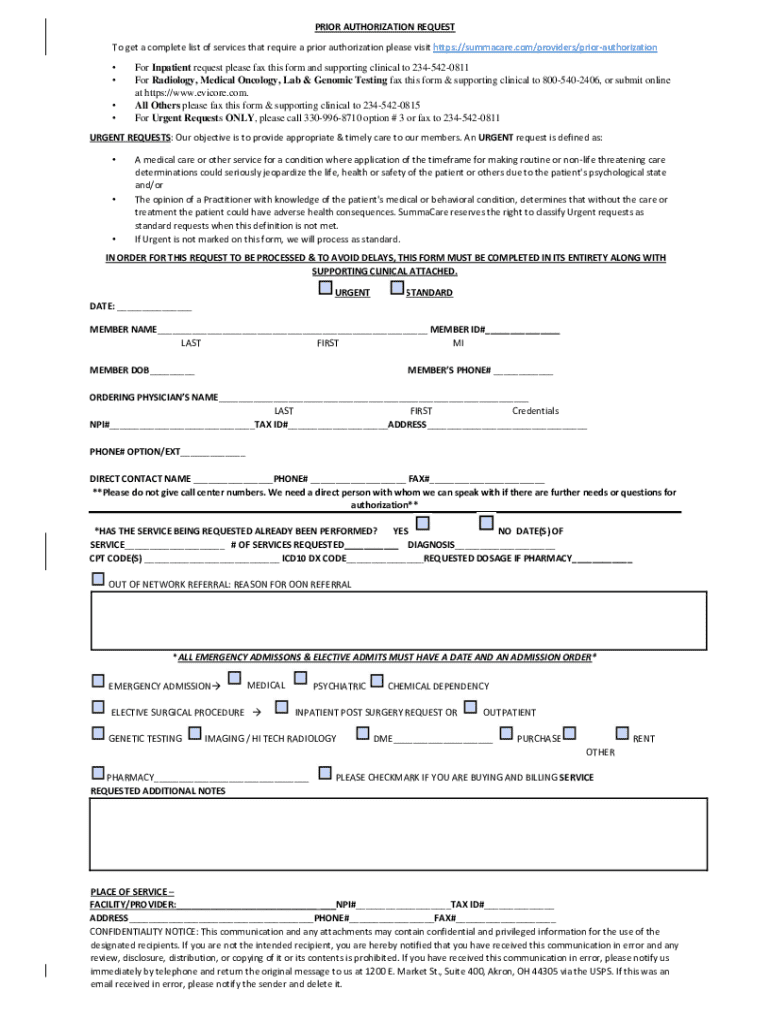
Comprehensive Guide to the Prior Authorization Request Form
Understanding prior authorization
Prior authorization is a critical process within the healthcare system where insurance companies require healthcare providers to obtain approval before a specific service or medication can be covered. This protocol ensures that the service is medically necessary and aligns with the healthcare insurance policy.
The importance of prior authorization cannot be understated. This mechanism helps control healthcare costs and promotes the use of effective treatments. For many patients, it can mean the difference between receiving timely treatment and facing delays due to administrative hurdles.
Overview of the prior authorization request form
The prior authorization request form serves as the formal document required by insurance providers to approve specific medical services. It standardizes the process, ensuring required information is collected efficiently.
Key components of the form typically include:
Different insurance providers may have variations of the form, reflecting specific requirements unique to their policies.
Step-by-step guide to completing the prior authorization request form
Completing the prior authorization request form can be streamlined by following a structured approach. Start by gathering required information to avoid delays.
Filling out each section accurately is crucial. Here are steps for completing the form:
Avoid common mistakes like incomplete information or use of incorrect codes, as these can lead to delays or denials.
Interactive tools for filling out the form
Platforms like pdfFiller offer interactive features to simplify the completion of the prior authorization request form. Users can benefit from auto-fill capabilities and guided filling processes.
Utilizing templates available on pdfFiller allows for quicker completions, particularly for forms that are frequently submitted.
Editing and signing the prior authorization request form
Once the form is completed, it may require modifications or additional information. pdfFiller grants users various editing options.
Moreover, the eSignature options available in pdfFiller provide a seamless way to authenticate documents legally.
The step-by-step signing process ensures users can easily complete this requirement without difficulty.
Submission process for the prior authorization request form
Submitting the completed prior authorization request form requires attention to detail. It is essential to understand the specific channels for each insurance provider.
After submitting, tracking the status of the request is vital. Each provider has its own system for updating the status, and responses may vary based on approved or denied requests.
Managing and storing your prior authorization request forms
Organizing submitted forms is essential for efficient healthcare management. With pdfFiller, users can easily manage submissions in a centralized location.
Troubleshooting common issues with prior authorization requests
Occasionally, requests may be denied, and understanding the reasons behind it can facilitate a smoother appeal process. Common reasons include insufficient medical justification or incorrect coding.
After receiving a denial, providers can appeal the decision by resubmitting additional documentation that addresses the identified issues. pdfFiller offers support resources for navigating this process effectively.
Additional features of pdfFiller for document management
pdfFiller not only simplifies filling out the prior authorization request form but also offers extensive features for document management.
Enhancing your document management experience
Transitioning from paper to a digital workflow using pdfFiller brings forth numerous advantages. It saves time, reduces errors, and enhances overall efficiency in managing healthcare documents.
Continuous updates on related topics via pdfFiller assist users in staying informed about new requirements or changes in processes related to prior authorizations.
For any questions or support needs, pdfFiller offers customer support and FAQs to assist users in optimizing their document management experience.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit prior authorization request straight from my smartphone?
How do I fill out prior authorization request using my mobile device?
Can I edit prior authorization request on an Android device?
What is prior authorization request?
Who is required to file prior authorization request?
How to fill out prior authorization request?
What is the purpose of prior authorization request?
What information must be reported on prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.