Get the free Multiple SclerosisPonvory Prior Authorization Policy
Get, Create, Make and Sign multiple sclerosisponvory prior authorization



How to edit multiple sclerosisponvory prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out multiple sclerosisponvory prior authorization

How to fill out multiple sclerosisponvory prior authorization
Who needs multiple sclerosisponvory prior authorization?
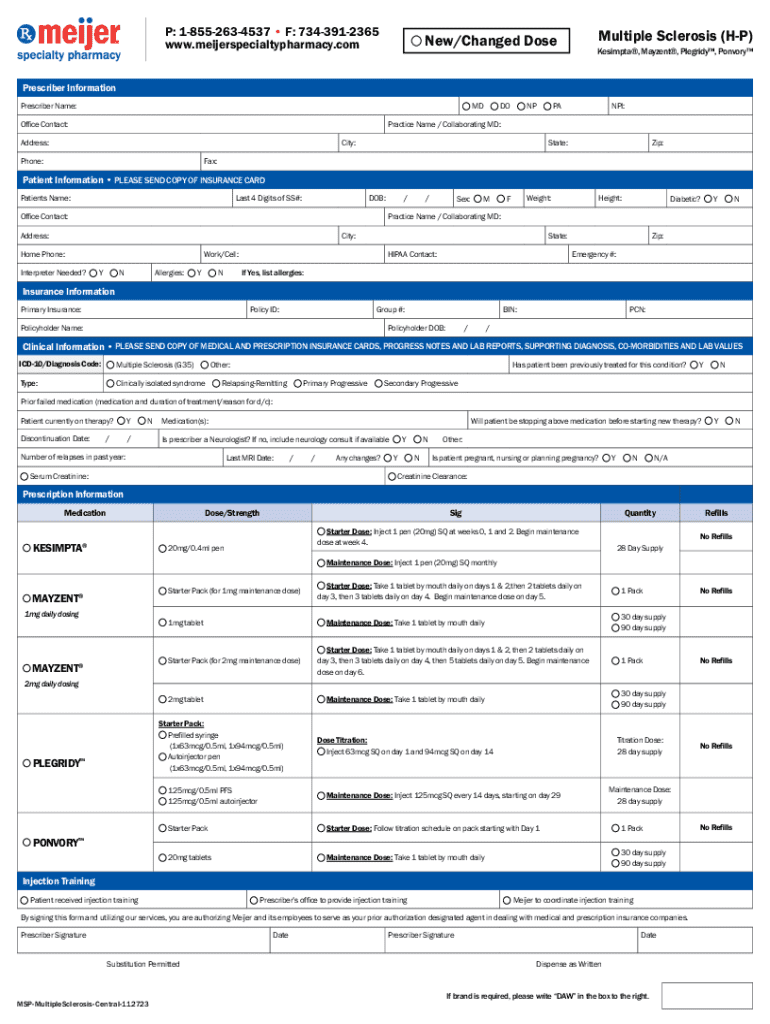
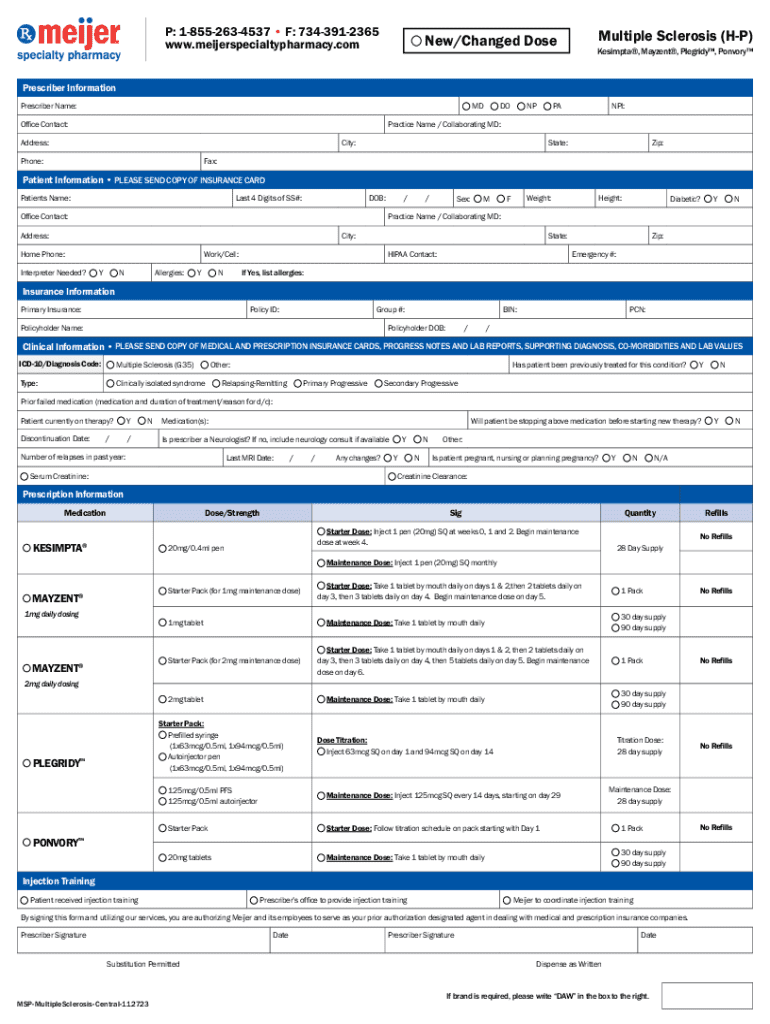
Navigating the Multiple Sclerosis Ponvory Prior Authorization Form: A Comprehensive Guide
Overview of Ponvory and its necessity
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, leading to a range of symptoms such as fatigue, mobility issues, cognitive difficulties, and more. As MS progresses, individuals often seek effective treatment options to manage their symptoms and maintain their quality of life. Ponvory (ponesimod) has emerged as a significant treatment for relapsing forms of MS, offering patients hope through its mechanism that selectively targets lymphocytes to reduce inflammation.
The journey to obtaining Ponvory typically begins with a prior authorization process. This step is essential for ensuring that the prescribed treatment is covered by insurance, as it confirms the medical necessity of the medication based on an individual's specific health needs and circumstances. Understanding this process could be key to securing timely access to Ponvory.
Detailed guide to the Ponvory prior authorization form
The Ponvory prior authorization form is a critical document designed to facilitate the approval process for prescribing Ponvory to patients. This form is submitted to insurance providers and plays a key role in determining coverage for the medication. Within this form, healthcare providers must provide pertinent information about the patient's medical condition and the rationale behind choosing Ponvory as a treatment option.
Typically, the Ponvory prior authorization form will require details such as the patient's demographics, including full name and date of birth, as well as the prescriber’s information. Additionally, a section would likely exist for outlining medical necessity, where the physician justifies why Ponvory is the appropriate choice for the patient based on their MS diagnosis and treatment history.
Step-by-step instructions for completing the form
Completing the Ponvory prior authorization form requires careful preparation and accurate information. Start by gathering all necessary details such as health insurance information, patient demographics, and the individual's medical history related to Multiple Sclerosis. This foundational information is crucial to ensure a smooth submission process and reduce the likelihood of delays.
When filling out the form, it's helpful to approach it section by section. Here's a breakdown of what each section typically entails:
Finally, ensure you accurately complete the signing and date section. This step is crucial for validity, as insurance companies require proper documentation to process the authorization request.
Tips for submitting the Ponvory prior authorization form
After completing the Ponvory prior authorization form, it's important to follow submission best practices. Begin by thoroughly reviewing the document for accuracy and completeness. Any errors or incomplete information can lead to delays or denials in coverage. Ensure that all required documentation is attached, including any medical records or previous treatment details that may support the authorization.
Consider the submission methods you have available:
Choosing the right submission method can significantly impact the speed and success of your authorization request.
What to expect after submission
Once the Ponvory prior authorization form is submitted, it enters the review phase of the approval process. Typically, healthcare providers will receive a decision from the insurance company within a few days to a couple of weeks. During this time, the authorization may either be approved, denied, or require additional information.
If approved, you’ll receive notification, allowing you to move forward with obtaining Ponvory through your pharmacy or healthcare provider. However, if a denial occurs, it’s vital to understand the reasons behind it, which can often include lack of documentation or failure to meet medical necessity criteria.
Addressing denials involves appealing the decision through your insurance provider, which may require resubmitting the form with additional information or clarifying the medical necessity of Ponvory.
Tools and resources to aid the process
pdfFiller stands out as a valuable tool for navigating the Ponvory prior authorization form process. Its features facilitate a seamless experience for completing, editing, and managing this document, providing users with the ability to eSign and securely share the authorization form. These capabilities streamline the submission process and enhance overall efficiency.
In addition, pdfFiller offers interactive tools designed to help users manage various prior authorization forms. With templates available for similar requests and easy sharing options for healthcare providers and patients, pdfFiller empowers individuals to approach the prior authorization process with confidence and ease.
Frequently asked questions (FAQs)
Navigating the Ponvory prior authorization process can prompt several questions, particularly for those unfamiliar with the system. Here are some common questions and their answers.
Additional considerations
When going through the Ponvory prior authorization process, it's important to keep in mind that insurance plans can vary significantly in their requirements. Different insurers may have distinct criteria and forms, which can impact the approval process, highlighting the importance of working closely with your healthcare provider throughout.
Furthermore, staying informed about any recent changes in treatment guidelines or protocols related to MS can enhance the chances of successful authorization, ensuring that the treatment is aligned with current best practices. Regular communication with your provider can provide critical updates that may affect your treatment plan.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my multiple sclerosisponvory prior authorization in Gmail?
How can I send multiple sclerosisponvory prior authorization to be eSigned by others?
How do I edit multiple sclerosisponvory prior authorization straight from my smartphone?
What is multiple sclerosis Ponvory prior authorization?
Who is required to file multiple sclerosis Ponvory prior authorization?
How to fill out multiple sclerosis Ponvory prior authorization?
What is the purpose of multiple sclerosis Ponvory prior authorization?
What information must be reported on multiple sclerosis Ponvory prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.