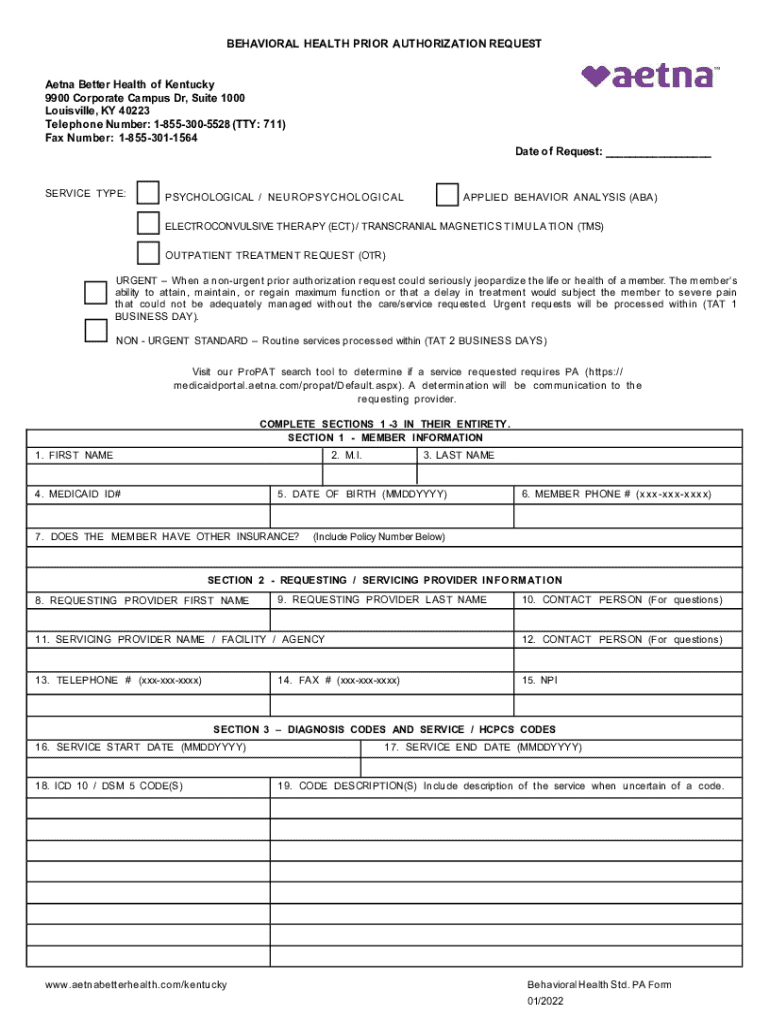
Get the free Behavioral Health Prior Authorization Request
Get, Create, Make and Sign behavioral health prior authorization
How to edit behavioral health prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out behavioral health prior authorization
How to fill out behavioral health prior authorization
Who needs behavioral health prior authorization?
Behavioral Health Prior Authorization Form: A How-to Guide
Understanding the behavioral health prior authorization process
Prior authorization is a critical process in the healthcare system that requires providers to obtain approval from an insurance company before delivering certain services. This step is particularly important in behavioral health, where specialized treatments often necessitate careful evaluation to ensure necessity and cost-effectiveness. Insurance providers commonly require prior authorization for various mental health services, ranging from therapy sessions to medications, ensuring that patients receive appropriate care without incurring unnecessary expenses.
Behavioral health prior authorization serves multiple purposes, including managing healthcare costs and ensuring that providers adhere to evidence-based treatment protocols. Common insurance requirements typically specify the type of information needed, such as diagnostic codes, treatment modalities, and expected outcomes. Awareness of these requirements is crucial for both providers and patients to navigate the authorization process effectively.
Key components of the behavioral health prior authorization form
A well-structured behavioral health prior authorization form consists of several essential components that facilitate thorough evaluation and approval for services. Understanding these sections is vital for completing the form accurately.
Step-by-step instructions for completing the form
Completing a behavioral health prior authorization form can be straightforward if you follow a clear set of steps. Let’s break down the process into manageable stages.
Submitting the behavioral health prior authorization form
Once the behavioral health prior authorization form is completed, the next step is submission. Understanding the recommended submission methods can ease this process significantly.
Handling denials and appeals
Despite best efforts, some prior authorization requests may be denied. Understanding the reasons for denial and the appeals process can empower providers to advocate for their patients effectively.
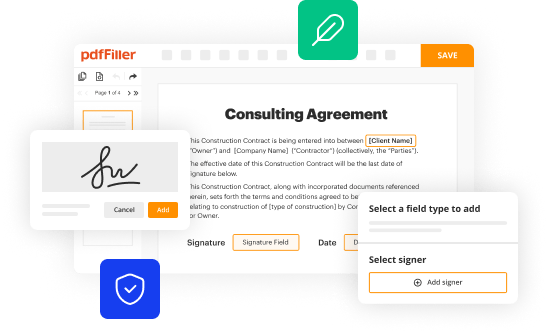
Utilizing pdfFiller for your behavioral health forms
pdfFiller offers an array of features tailored to streamline the completion and management of behavioral health forms. Utilizing their platform can simplify many aspects of the prior authorization process.
Best practices for efficient prior authorization management
Adopting best practices in managing the behavioral health prior authorization process can significantly enhance efficiency and accuracy.
Frequently asked questions (FAQs)
In navigating the behavioral health prior authorization landscape, several common questions arise that can be vital for providers and patients.
Real-life case studies
Examining real-life case studies provides insight into the practical application of behavioral health prior authorization processes, revealing the dramatic impact they can have on patient care.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit behavioral health prior authorization online?
How can I edit behavioral health prior authorization on a smartphone?
Can I edit behavioral health prior authorization on an iOS device?
What is behavioral health prior authorization?
Who is required to file behavioral health prior authorization?
How to fill out behavioral health prior authorization?
What is the purpose of behavioral health prior authorization?
What information must be reported on behavioral health prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.