Get the free Medication Prior Authorization Request Form
Get, Create, Make and Sign medication prior authorization request



How to edit medication prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medication prior authorization request

How to fill out medication prior authorization request
Who needs medication prior authorization request?
Medication Prior Authorization Request Form: A Comprehensive How-to Guide
Understanding medication prior authorization
Medication prior authorization is a crucial process within healthcare, designed to manage and control the costs of beneficial medications. Prior authorization acts as a gatekeeping mechanism, requiring healthcare providers to obtain approval from a patient's insurance company before a specific medication is covered. This process holds both benefits and challenges for patients and insurers, ensuring that prescribed medications meet clinical criteria while also managing overall healthcare expenditures.
The importance of medication prior authorization is twofold. For patients, it can mean the difference between receiving necessary treatments or being confronted with unexpected costs. For insurers, it aids in the regulation of drug utilization, encourages the utilization of less expensive alternatives, and ensures that treatments align with established guidelines. In many cases, prior authorization is essential, especially for high-cost or potentially harmful medications.
When is prior authorization needed?
Prior authorization is typically required in various scenarios. Common instances include when prescribed medications are newly approved by the FDA, identified as high-cost medications, or considered non-formulary by the insurance provider. Additionally, treatments for certain chronic conditions, such as rheumatoid arthritis or cancer therapies, frequently necessitate authorization.
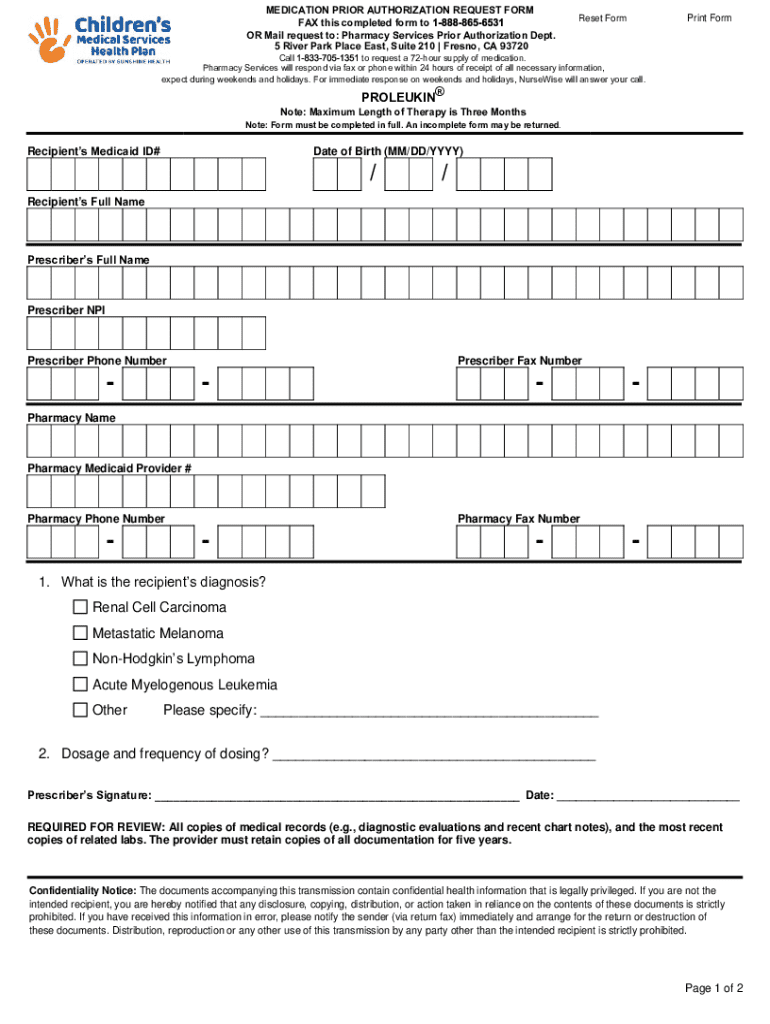
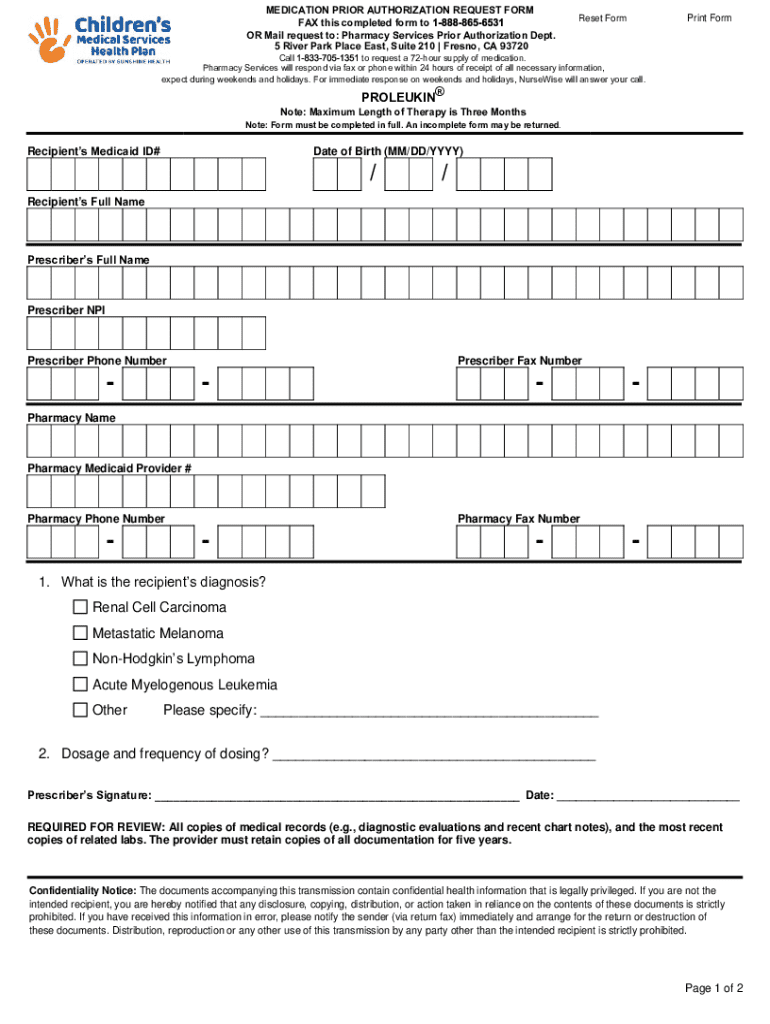
The role of the medication prior authorization request form
The medication prior authorization request form plays a fundamental role in the authorization process. It serves as a structured document that healthcare providers must complete and submit to the insurance company to facilitate the approval of prescribed medications. This form acts as a formal request to the insurer, outlining necessary details to determine whether the treatment aligns with established criteria.
Essential components of the medication prior authorization request form include patient identification, medication details, diagnosis codes, and any relevant medical history. Accurate information is crucial, as incomplete or incorrect data can lead to delays or denials, impacting timely access to medications crucial for patient care.
How to fill out the medication prior authorization request form
Filling out the medication prior authorization request form can be straightforward if approached methodically. Follow these step-by-step instructions to ensure accuracy and completeness:
Common mistakes to avoid include leaving sections blank, providing incomplete medication histories, or misunderstanding the documentation needed to support the medical necessity of treatment. Take your time while completing the form, as errors can lead to frustrating delays that compromise patient care.
Editing and managing your request form
Using pdfFiller can greatly enhance the ease of managing your medication prior authorization request forms. This platform offers robust editing tools that facilitate seamless creation and alteration of forms, ensuring that inaccuracies can be corrected quickly and efficiently.
Best practices for document management include organizing forms within designated folders, naming them for easy retrieval, and maintaining an updated log of submissions. Features like cloud storage enable you to access your documents anytime, anywhere, empowering you to manage requests on-the-go.
Signature and submission process
Once your medication prior authorization request form is completed, the eSigning process can be accomplished using pdfFiller. This straightforward method allows for quick and secure signing of documents, eliminating the need for printing and scanning.
Submission of your request can take several forms, including online uploads, faxing, or mailing the document to the insurer. Each method has its advantages, but using an electronic method often ensures quicker processing times. Always confirm the submission method recommended by the insurance provider and maintain a record of the submission for follow-up purposes.
After submission: what to expect
After submission of your medication prior authorization request form, the review process begins. Insurers typically evaluate requests based on clinical guidelines and protocols. Expect that there may be periods of waiting as the insurer assesses the necessity and appropriateness of the requested medication. Generally, responses can come back in various formats, such as full approvals, denials, or requests for additional information.
In case of a denial, it’s crucial to take proactive steps. Understand that denials are not final; you can request a detailed explanation for the denial and initiate an appeal process. The importance of having a clear plan for appeals cannot be overstated, as it may eventually result in authorization after further justification is provided.
Frequently asked questions (FAQs)
Those navigating the medication prior authorization request form might have several questions. Common inquiries include timelines for response from insurers, potential costs associated with medications pending prior authorization, and understanding what constitutes a medical necessity. Familiarizing yourself with your insurance provider's standard procedures can ease this process.
Additionally, seeking technical support from pdfFiller can be invaluable. Access their resources or customer support for assistance with form completion, document management, and using features effectively to streamline requests.
Tips for effective collaboration
Effective collaboration with healthcare providers is essential during the medication prior authorization process. Open communication with physicians and pharmacists not only ensures that everyone is aware of the patient's treatment plan but also assists in gathering necessary information to support the authorization request.
Using pdfFiller allows teams to share and collaborate on forms efficiently. With the platform's collaborative features, multiple stakeholders can contribute to form completion without the confusion of multiple document versions. This can significantly streamline the process and reduce turnaround times.
Leveraging technology for a seamless experience
The features of pdfFiller significantly simplify authorization requests, providing users with a versatile, cloud-based document management solution. These technologies offer mobility, allowing users to access their documents from different locations seamlessly, which is particularly beneficial for healthcare providers with busy schedules.
Moreover, integrating pdfFiller with other healthcare management systems can enhance workflow efficiency. It ensures that all necessary documentation is easily accessible in one place, ultimately leading to improved patient care and quicker resolution of authorization requests.
Conclusion
Managing the medication prior authorization process effectively can empower both patients and healthcare providers. A well-structured process not only facilitates medication access for patients but also supports insurers in maintaining cost control. By utilizing tools like pdfFiller, users can take advantage of a comprehensive document management platform that streamlines forms and approval workflows.
The future of medication prior authorization looks promising with the advancements in technology. As digital solutions continue to evolve, they promise to enhance the efficiency and ease of the authorization process, reducing administrative burdens and improving patient experiences in the healthcare landscape.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my medication prior authorization request in Gmail?
How can I get medication prior authorization request?
How can I edit medication prior authorization request on a smartphone?
What is medication prior authorization request?
Who is required to file medication prior authorization request?
How to fill out medication prior authorization request?
What is the purpose of medication prior authorization request?
What information must be reported on medication prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.