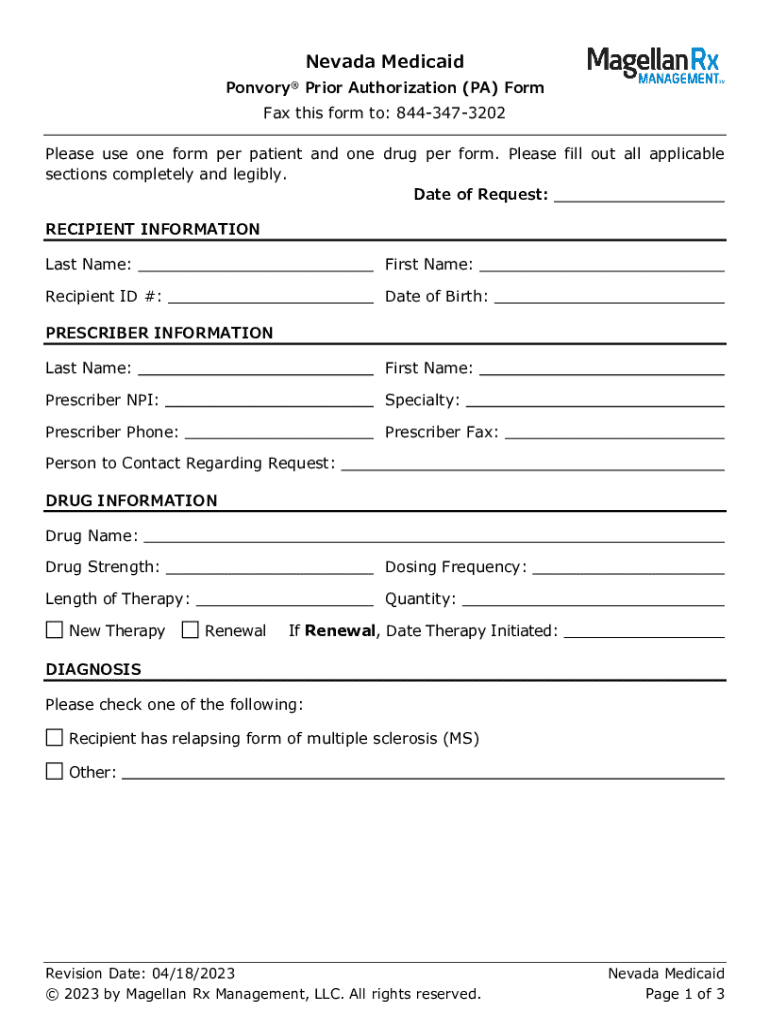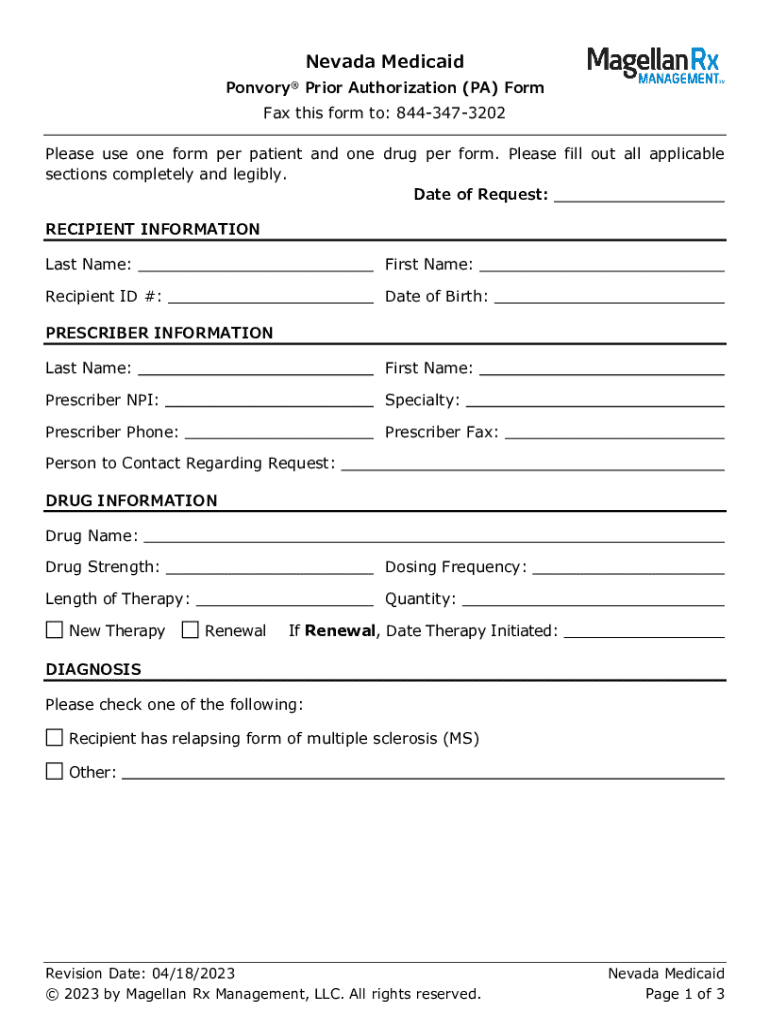
Get the free Nevada Medicaid Ponvory® Prior Authorization (pa) Form
Get, Create, Make and Sign nevada medicaid ponvory prior



How to edit nevada medicaid ponvory prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nevada medicaid ponvory prior

How to fill out nevada medicaid ponvory prior
Who needs nevada medicaid ponvory prior?
Navigating the Nevada Medicaid Ponvory Prior Form: A Complete Guide
Understanding the Nevada Medicaid Ponvory Program
Ponvory (ponsinaran) is a medication designed for the treatment of multiple sclerosis, helping to reduce the frequency and severity of relapses. In Nevada, the Medicaid program recognizes the importance of this treatment and thus offers Ponvory coverage to eligible residents. However, accessing Ponvory through Nevada Medicaid is contingent upon obtaining prior authorization, a crucial step that ensures the medication is medically necessary for the individual patient.
Eligibility for Nevada Medicaid's coverage of Ponvory primarily involves meeting specific medical criteria, which is outlined by the state. Patients must possess a documented diagnosis of relapsing forms of multiple sclerosis (RMS) and have demonstrated that other first-line therapies have either failed or are not suitable for them. This framework allows the Medicaid program to maintain a focus on medical necessity, ensuring that patients receive treatments tailored to their unique health needs.
The importance of the prior authorization process
Prior authorization serves as a gatekeeper within healthcare, requiring that certain medications or treatments receive approval before being dispensed. For the Nevada Medicaid Ponvory program, this process is designed to evaluate the necessity of the medication for each patient based on established medical guidelines. This step is vital for both the patients and the Medicaid program, ensuring efficient use of healthcare resources.
Many patients may harbor misconceptions about the prior authorization process. Some believe that it solely delays treatment, while others think that their providers may not advocate strongly enough on their behalf. In reality, prior authorization is a standardized procedure meant to promote responsible prescribing, which ultimately leads to better patient outcomes. It's essential for patients and their caregivers to understand how to navigate this process effectively to minimize potential barriers to treatment.
Step-by-step guide to completing the Ponvory prior authorization form
Accessing the form
To begin the process for the Nevada Medicaid Ponvory prior authorization, you first need to locate the appropriate form. This can typically be found on the Nevada Medicaid website, where it is available in various formats, including a downloadable PDF and an online submission option.
Required information on the form
Filling out the prior authorization form requires several key pieces of information, including:
Instructions for completing each section
When filling out the prior authorization form, it is important to carefully adhere to the guidelines provided by Nevada Medicaid. Accurately entering patient information is crucial, as discrepancies can lead to delays or denials. Similarly, ensure that the medical history is both detailed and relevant, clearly outlining why Ponvory is not just a treatment option, but a medical necessity for the patient.
Common errors to avoid
Despite best efforts, applicants often make mistakes that can hinder their application process. Common pitfalls include:
Submitting the prior authorization form
Submission methods
Once the prior authorization form is completed, it must be submitted for review. Nevada Medicaid offers multiple submission methods, allowing for flexibility. Patients can choose to submit their requests online through the Nevada Medicaid portal, which is often the quickest way to receive confirmation. Alternatively, forms can be sent via mail, where it's advisable to use certified mail to track the submission.
Tracking your application
After submission, staying informed about the application's progress is crucial. Patients should follow up on their request status within a week or two, as prior authorization reviews typically take a few business days. Eagerly checking the online portal or calling the Medicaid office can help in understanding if further information is needed or if a decision has been reached.
What happens after submission?
Following the submission of the Ponvory prior authorization form, Nevada Medicaid undertakes a review process. This evaluation determines whether the requested treatment is in line with the established medical necessity criteria. The outcomes can result in one of three possibilities:
In the case of a denial, understanding the appeals process is vital. Patients and their providers can work together to address the reasons for denial and resubmit the application with additional supporting documentation if needed.
Frequently asked questions about the Ponvory prior authorization process
Patients often have questions regarding the prior authorization process for Ponvory through Nevada Medicaid. Some of the most commonly asked questions include:
Leveraging pdfFiller for efficient document management
Editing the Ponvory prior authorization form
Using pdfFiller, applicants can easily edit the Ponvory prior authorization form. The platform provides tools that allow users to fill out the form directly online, streamlining the completion process while ensuring all necessary information is included. Users can save templates for future requests, simplifying repeated submissions.
eSigning and collaborating on documents
In addition to filling out forms, pdfFiller facilitates the secure electronic signing of documents. This feature ensures that all necessary signatures are captured promptly, eliminating delays associated with mailing physical documents. Furthermore, the collaboration tools allow caregivers and healthcare providers to work together, ensuring comprehensive and accurate submissions.
Organizing and managing your documents
pdfFiller offers a cloud-based platform where users can organize all their important documents in one place. This approach allows for easy access from anywhere, ensuring that patients and providers can manage documentation efficiently. Storing prior authorization forms and related information in a single platform mitigates the risk of misplacement and enhances overall workflow.
Conclusion
The process for obtaining the Nevada Medicaid Ponvory prior authorization may seem daunting, but with the right tools and understanding, it can be navigated smoothly. Utilizing pdfFiller for form management not only simplifies the application process but also enhances communication between patients and their healthcare providers. By engaging proactively with the prior authorization process, patients can focus on their health and treatment with greater peace of mind.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my nevada medicaid ponvory prior directly from Gmail?
How do I make edits in nevada medicaid ponvory prior without leaving Chrome?
How do I edit nevada medicaid ponvory prior on an Android device?
What is nevada medicaid ponvory prior?
Who is required to file nevada medicaid ponvory prior?
How to fill out nevada medicaid ponvory prior?
What is the purpose of nevada medicaid ponvory prior?
What information must be reported on nevada medicaid ponvory prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.