Get the free Nemluvio® (nemolizumab-ilto) Prior Authorization Form
Get, Create, Make and Sign nemluvio nemolizumab-ilto prior authorization



How to edit nemluvio nemolizumab-ilto prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nemluvio nemolizumab-ilto prior authorization

How to fill out nemluvio nemolizumab-ilto prior authorization
Who needs nemluvio nemolizumab-ilto prior authorization?
Nemluvio Nemolizumab-Ilto Prior Authorization Form: A Comprehensive Guide
Understanding the Nemluvio Nemolizumab-Ilto
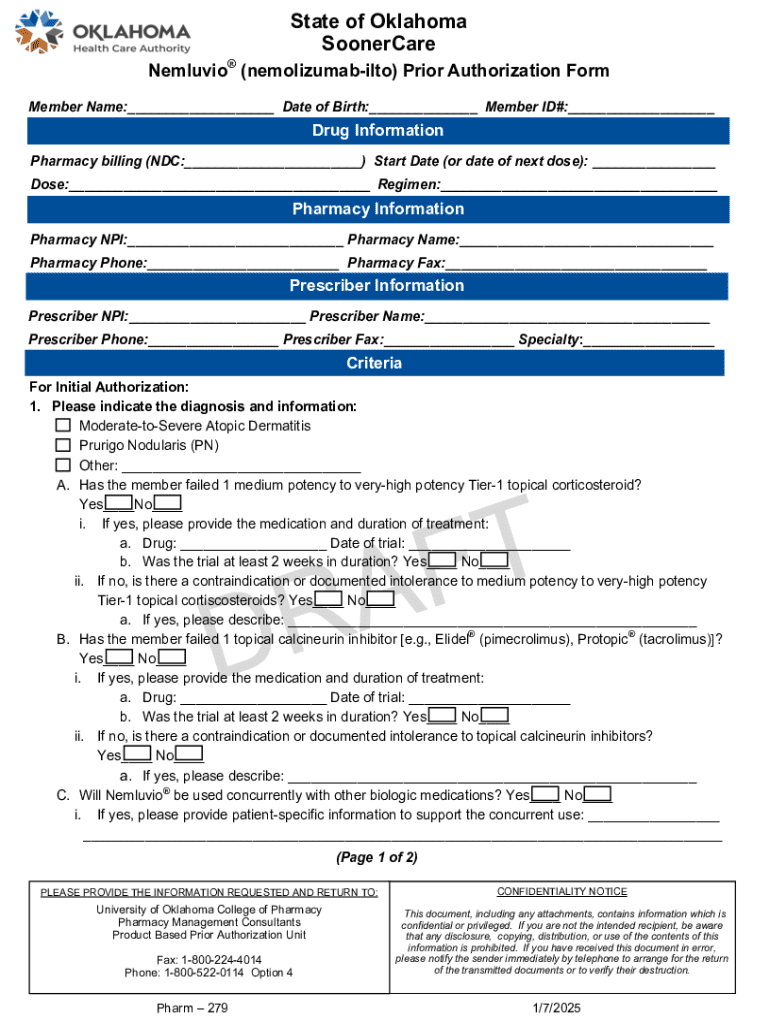
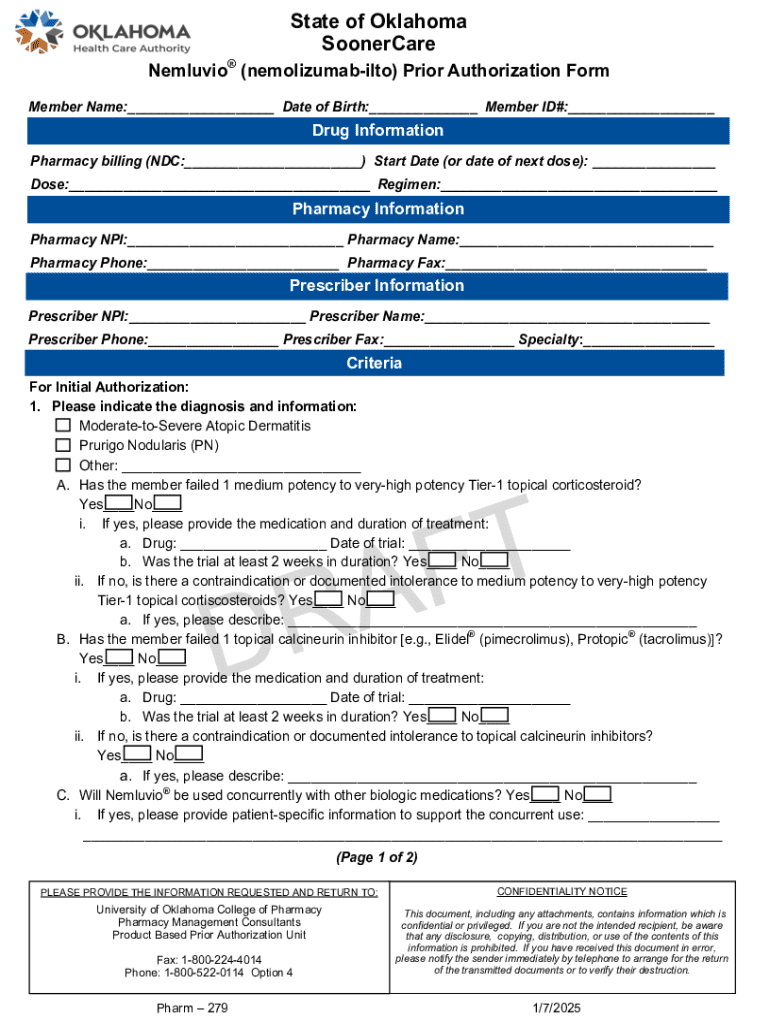
Nemluvio (nemolizumab-ilto) is a monoclonal antibody that has been developed for the treatment of moderate to severe atopic dermatitis, particularly in patients who are not adequately controlled by topical therapies. Its therapeutic use extends to other immunological conditions, showcasing its versatility in targeting inflammation pathways. The effective use of Nemluvio hinges upon efficient prior authorization from insurance providers, ensuring that patients receive medications that are both necessary and appropriate for their conditions.
Prior authorization is a crucial process that safeguards against unnecessary treatments and expenses, enabling healthcare providers to present a strong case for the necessity of Nemluvio. It's designed to ensure that patients meet specific criteria before the drug can be dispensed, ultimately protecting both the healthcare system and the patient.
Eligibility criteria for Nemluvio treatment
To qualify for Nemluvio treatment, patients typically must have a diagnosis of moderate to severe atopic dermatitis or another relevant condition. Common eligibility criteria may include:
Required documentation for eligibility verification typically includes detailed clinical notes, treatment history, and potentially lab results, all of which reinforce the need for the prescribed medication.
Navigating the prior authorization process
Understanding what prior authorization entails is vital for patients and providers alike. This process necessitates that healthcare providers secure approval from insurance companies before prescribing Nemluvio, ensuring that the proposed medical treatment meets specific policy criteria. This step is essential not just for the patient but also for the healthcare provider to avoid unexpected out-of-pocket costs.
The steps involved in successfully navigating the prior authorization process are as follows:
Filling out the Nemluvio prior authorization form using pdfFiller
Accessing the Nemluvio prior authorization form through pdfFiller is straightforward. Users can find the necessary forms easily by searching in their document management interface. Here’s a quick guide on how to edit the form effectively:
These user-friendly tools enhance the submission process, allowing users to collaborate seamlessly with healthcare professionals on the document. Making comments or adding notes for clarity can also help the reviewing insurance representatives.
Common challenges and solutions
The journey through the prior authorization process may not be devoid of challenges. Frequent issues encountered include missing documentation, which can delay approval, and errors in patient data entry that can lead to outright denials. To mitigate these risks, here are some solutions:
If there is a denial, understanding the reasons behind it is key. Reviewing the denial letter closely allows you to pinpoint what additional information is needed for an effective appeal. Steps to appeal a denial typically include gathering supplementary documentation and resubmitting the authorization request promptly.
Follow-up and next steps
Once the prior authorization request has been submitted, knowing how to track it is crucial. Most insurers provide a tracking system or online portal where you can check the status of your request. Typical processing times vary, generally taking anywhere from a few days to a couple of weeks, depending on the insurer.
After receiving approval, patients should coordinate with their healthcare provider regarding the next steps in beginning treatment. This includes scheduling an appointment to discuss how and when to start using Nemluvio, as well as any additional counseling on managing their condition effectively.
Leveraging pdfFiller for document management
pdfFiller empowers users to manage not just the Nemluvio prior authorization form but also any related medical documentation seamlessly from a single platform. With its cloud-based solution, individuals and teams can organize their medical documents effectively, ensuring they are easily accessible when needed.
Utilizing pdfFiller also involves understanding its comprehensive document management features, which include secure cloud storage, easy sharing options, and signature capabilities, all beneficial for managing healthcare documentation efficiently. Moreover, these features align with regulatory compliance, thereby aiding in maintaining security and confidentiality.
Testimonials and user experiences
Hearing success stories from others who successfully navigated the Nemluvio prior authorization process can be encouraging. Many patients have reported a smoother experience by leveraging pdfFiller’s capabilities, specifically highlighting its ease of use and ability to seamlessly collaborate with medical professionals.
Engaging with the pdfFiller community through forums and discussion boards has been beneficial for users looking to share personal experiences or seek guidance on document management solutions. This peer support can provide reassurance and practical advice on overcoming common hurdles faced during the authorization process.
Additional tips for a successful authorization process
In closing, maintaining organization is vital throughout the prior authorization process. Keeping all related documents, communication records, and other materials organized will ease the burden during the request phase. Patients and caregivers are encouraged to:
By integrating these strategies into their approach, patients can enhance their experience and improve the likelihood of speedy authorization for Nemluvio treatment.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit nemluvio nemolizumab-ilto prior authorization in Chrome?
How can I edit nemluvio nemolizumab-ilto prior authorization on a smartphone?
How do I fill out nemluvio nemolizumab-ilto prior authorization on an Android device?
What is nemluvio nemolizumab-ilto prior authorization?
Who is required to file nemluvio nemolizumab-ilto prior authorization?
How to fill out nemluvio nemolizumab-ilto prior authorization?
What is the purpose of nemluvio nemolizumab-ilto prior authorization?
What information must be reported on nemluvio nemolizumab-ilto prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.