Get the free Nonpreferred Drugs Prior Authorization of Benefits Form
Get, Create, Make and Sign nonpreferred drugs prior authorization



Editing nonpreferred drugs prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nonpreferred drugs prior authorization

How to fill out nonpreferred drugs prior authorization
Who needs nonpreferred drugs prior authorization?
Understanding the Nonpreferred Drugs Prior Authorization Form
Overview of nonpreferred drugs prior authorization
Nonpreferred drugs are those medications that are not included on a health insurance plan's list of covered drugs, commonly referred to as a formulary. These drugs typically have more expensive alternatives that insurers prefer to encourage the use of. The need for a prior authorization process for these medications serves a critical role in healthcare management. Prior authorization is a mechanism that requires healthcare providers to obtain approval before a specific medication or service is provided to the patient.
Nonpreferred drugs may become necessary in certain clinical situations, such as when a patient has previously tried and failed to respond to preferred alternatives. Understanding when these medications are imperative is crucial not only for compliance but also for optimal patient care.
Understanding the prior authorization process
The process of obtaining prior authorization for nonpreferred drugs involves several key steps that both prescribers and patients should understand thoroughly. The first step is initiating the request, which typically involves the prescriber contacting the insurance company to begin the authorization process.
Common reasons for prior authorization denials include lack of medical necessity and insufficient supporting information. It is vital for prescribers to provide comprehensive details to minimize the chances of rejection.
The role of nonpreferred drugs in treatment plans
Nonpreferred drugs often contrast with preferred drugs, which are generally more cost-effective and included in formularies. However, there are specific scenarios where nonpreferred drugs are warranted, such as when a patient exhibits an allergy to a component of a preferred medication or has unique health conditions that necessitate a specific drug choice.
In these cases, the utilization of nonpreferred medications becomes an essential component of a tailored treatment plan, ensuring better outcomes for patients despite the bureaucratic steps involved in obtaining the necessary approvals.
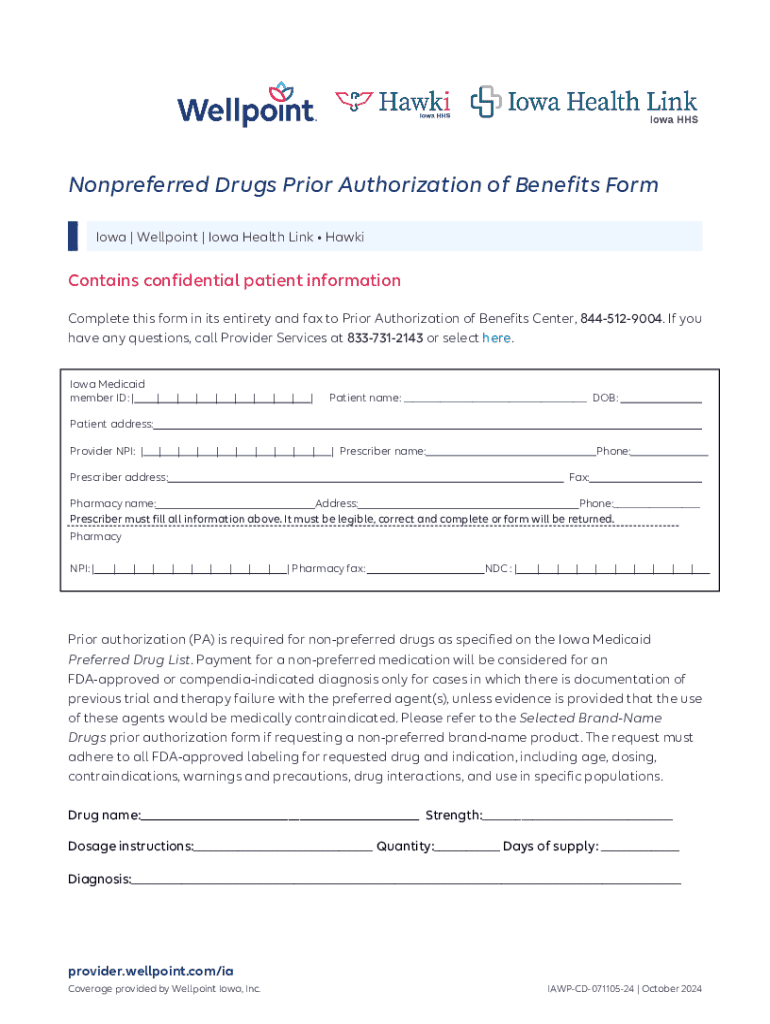
Detailed instructions for filling out the nonpreferred drugs prior authorization form
Filling out the nonpreferred drugs prior authorization form accurately is critical. The form generally requires various pieces of information to signify medical necessity effectively. Key details include patient demographics, prescriber information, and a thorough medical history with justification for prescribing the nonpreferred medication.
To ensure clarity and accuracy, be aware of common mistakes such as incorrect patient identifiers or missing supporting evidence. Providing robust case examples can also help guide form completion.
Tools available on pdfFiller for managing your prior authorization requests
Utilizing pdfFiller simplifies the task of managing your nonpreferred drugs prior authorization forms. This platform offers several interactive features to ease the editing and submission processes. With pdfFiller, users can efficiently fill out PDFs without hassle and utilize electronic signature capabilities for quicker processing.
The collaborative features of pdfFiller are also beneficial for teams, allowing real-time editing and input from different members involved in patient care.
Submitting the nonpreferred drugs prior authorization form
Once the prior authorization form for nonpreferred drugs has been completed, it must be submitted appropriately. There are several submission methods available, including online through various payer systems or offline by mailing the documents directly.
After submitting the request, prescribers should be aware of the typical timelines for decisions and follow-up procedures to check on the status of the authorization.
Troubleshooting and FAQs
Navigating the prior authorization process can come with its challenges, especially concerning delays in approvals or potential denials. Many healthcare providers face obstacles such as unclear communication from insurance companies or requests for additional information.
Frequently asked questions regarding nonpreferred drugs prior authorization often pertain to whether a resubmission is necessary after a denial or how to track the status of a request, highlighting the need for clarity in the process to ensure patient care is not hindered.
Best practices for prescribers and patients
Effective communication between prescribers, pharmacies, and payers is key to avoiding delays and misunderstandings throughout the prior authorization process. Strategies such as providing comprehensive documentation and maintaining open channels for questions can significantly enhance collaboration.
Patients also need education regarding nonpreferred drugs and the importance of adhering to the prior authorization process. Understanding the necessity of approvals can foster better adherence to treatment regimens.
Case studies: Success stories with nonpreferred drugs prior authorization
Real-life examples offer valuable insights into the challenges and triumphs of navigating prior authorizations for nonpreferred drugs. Observing the experiences of various patients can highlight effective strategies in obtaining approvals.
These success stories underscore the importance of persistence, communication, and the strategic use of documentation in gaining access to necessary medications.
Additional forms related to nonpreferred drugs and prior authorization
Various forms and supporting documentation may accompany the nonpreferred drugs prior authorization form. Understanding these additional needs can streamline the process significantly.
Furthermore, staying informed on state-specific guidelines and requirements will ensure compliance and smoother processing of requests.
Industry trends and future of prior authorization for nonpreferred drugs
The landscape of prior authorization is evolving, with emerging technologies streamlining processes and improving patient access to medications. Insurers are increasingly adopting innovative solutions that enhance efficiency in approvals and reduce turnaround times.
These trends indicate a shift towards optimizing the patient experience while maintaining cost control, promoting a more sustainable healthcare model.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out the nonpreferred drugs prior authorization form on my smartphone?
Can I edit nonpreferred drugs prior authorization on an Android device?
How do I fill out nonpreferred drugs prior authorization on an Android device?
What is nonpreferred drugs prior authorization?
Who is required to file nonpreferred drugs prior authorization?
How to fill out nonpreferred drugs prior authorization?
What is the purpose of nonpreferred drugs prior authorization?
What information must be reported on nonpreferred drugs prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.