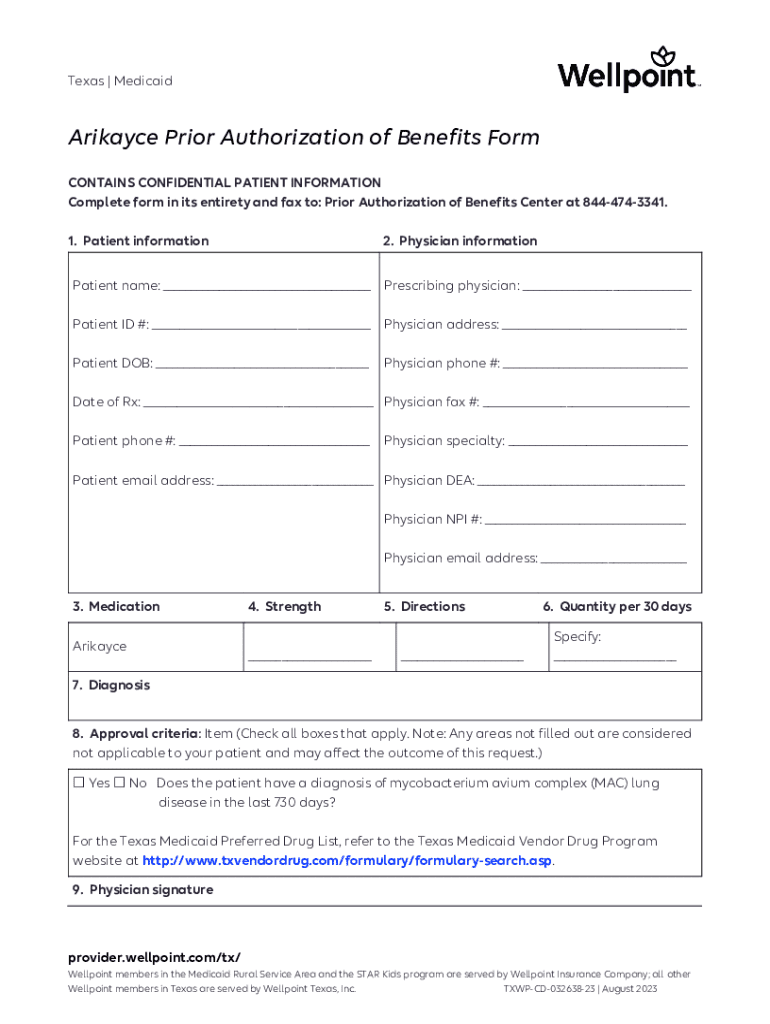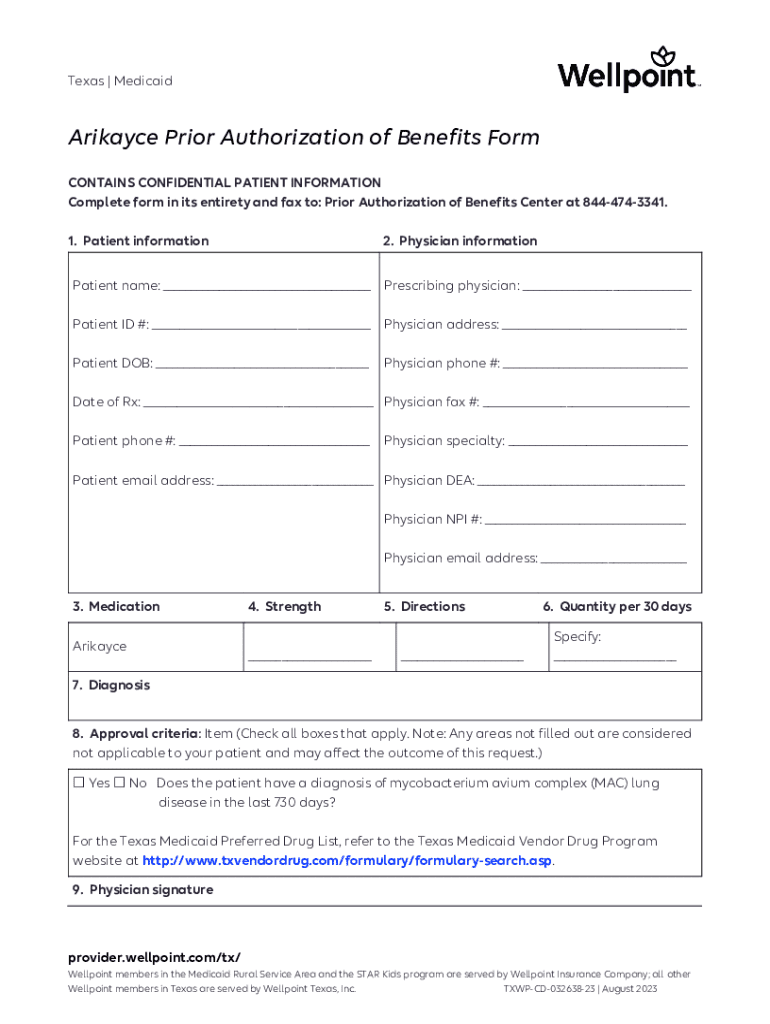
Get the free Arikayce Prior Authorization of Benefits Form
Get, Create, Make and Sign arikayce prior authorization of
How to edit arikayce prior authorization of online
Uncompromising security for your PDF editing and eSignature needs
How to fill out arikayce prior authorization of
How to fill out arikayce prior authorization of
Who needs arikayce prior authorization of?
Arikayce prior authorization of form: A comprehensive guide
Understanding prior authorization for Arikayce
Prior authorization is an essential part of the healthcare process, especially for high-cost medications like Arikayce. It is a requirement set by insurance companies to ensure that specific criteria are met before they approve coverage for a treatment. The purpose of prior authorization is to assess the medical necessity of treatments to prevent unnecessary expenses for both the insurer and the patient.
In the case of Arikayce, which is used to treat Mycobacterium avium complex (MAC) lung disease, prior authorization is crucial. It impacts patient access significantly, as insurance companies want to ensure that patients meet clinical guidelines before approving treatment. Key stakeholders in this process include patients who require the medication, healthcare providers who submit the necessary documentation, and insurers who review requests.
Initiating the prior authorization process
Starting the prior authorization process for Arikayce can seem daunting, but breaking it down into manageable steps can streamline the experience. Here’s a step-by-step guide to initiate the process effectively.
Common pitfalls during this process include submitting incomplete forms or outdated medical records. Patients and providers should communicate effectively to prevent these issues from arising.
Filling out the Arikayce prior authorization form
When completing the Arikayce prior authorization form, attention to detail is paramount. Start by entering patient details, such as name, contact information, and health plan ID. Ensure that the patient's medical history closely relates to the need for Arikayce.
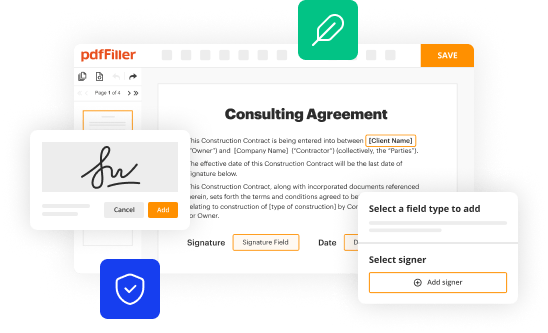
Information about prior treatments and any documented interactions with healthcare providers should also be included. Furthermore, utilizing tools like pdfFiller can help streamline this process. With pdfFiller, users can easily edit, sign, and save documents, reducing the likelihood of errors in submission.
Submitting the prior authorization request
After completing the Arikayce prior authorization form, the next step is submission. There are several methods to submit your request, including online portals, faxing documents, or mailing them directly to the insurance company.
Each method has its pros and cons, but submitting via an online portal can often provide immediate confirmation of receipt. Tracking submission status is essential; most insurers offer a way to check your claim or authorization status online. Ensure all documentation supports your case, as thorough documentation can significantly improve approval chances.
Understanding insurance coverage for Arikayce
Insurance coverage for Arikayce can vary widely based on individual plans and the specifics of the patient's medical history. Most private insurance plans include coverage for Arikayce, although prior authorization is generally required. Understanding these nuances is vital in navigating coverage.
For those without insurance or with limited coverage, financial assistance options exist, including patient assistance programs offered by pharmaceutical companies. Engaging with a social worker or case manager can also uncover additional resources to help alleviate financial burdens.
Navigating challenges in the prior authorization approval process
The prior authorization approval process can pose various challenges, such as common reasons for denial, including insufficient supporting documents or failure to meet clinical guidelines. Understanding these potential pitfalls can empower patients and providers alike.
If faced with a denial, strategies for appealing the decision include gathering additional supporting information, providing a letter of medical necessity from the prescribing physician, and clearly outlining why Arikayce is essential for the patient's health. Healthcare providers play a crucial role in this process, as their advocacy can significantly influence the outcome of an appeal.
Support programs for patients
Navigating the complexities of Arikayce can be less daunting with the help of support programs like inLighten Patient Support. These programs offer financial assistance, educational resources, and guidance throughout the prior authorization process.
Enrolling in such support programs can also provide patients with access to a network of healthcare professionals who can answer questions and expedite the authorization process. Contacting program representatives for assistance can ensure patients receive the necessary treatment quickly.
Maintaining continuous access to Arikayce
Once authorization for Arikayce is granted, maintaining continuous access is crucial. Transitioning to ongoing therapy may require periodic re-authorizations, particularly if there are changes in treatment plans or insurance.
To ensure an uninterrupted supply of medication, patients should stay proactive. This includes keeping an open line of communication with healthcare providers and insurers to verify coverage and renewal timelines.
Additional considerations for patients
Changing insurance plans can impact prior authorization requirements for Arikayce, making it essential for patients to understand their new benefits. Additionally, patients should stay informed about potential updates to coverage policies that could affect access.
Continuous education related to Arikayce and its availability through reliable healthcare resources is invaluable for patients. Awareness of the latest guidelines and support tools can empower proactive management of their treatment journey.
Using tools and resources effectively
Leveraging tools such as pdfFiller can significantly enhance the experience of managing the Arikayce prior authorization process. pdfFiller enables users to create, edit, eSign, and share documents seamlessly online.
Features like remote access to templates and documents, along with collaborative capabilities, make it easier for patients and providers to work together efficiently. This functionality integrates with healthcare workflows, ensuring that all necessary forms are filled out correctly and submitted promptly for best results.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete arikayce prior authorization of online?
Can I create an eSignature for the arikayce prior authorization of in Gmail?
How can I fill out arikayce prior authorization of on an iOS device?
What is arikayce prior authorization of?
Who is required to file arikayce prior authorization of?
How to fill out arikayce prior authorization of?
What is the purpose of arikayce prior authorization of?
What information must be reported on arikayce prior authorization of?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.