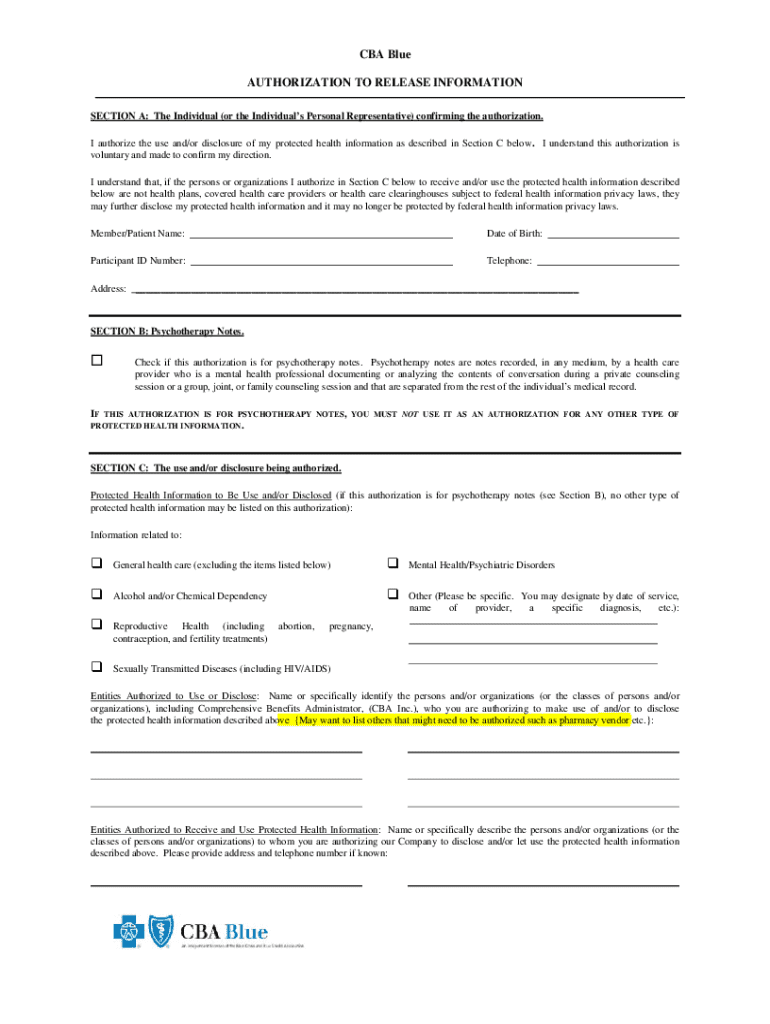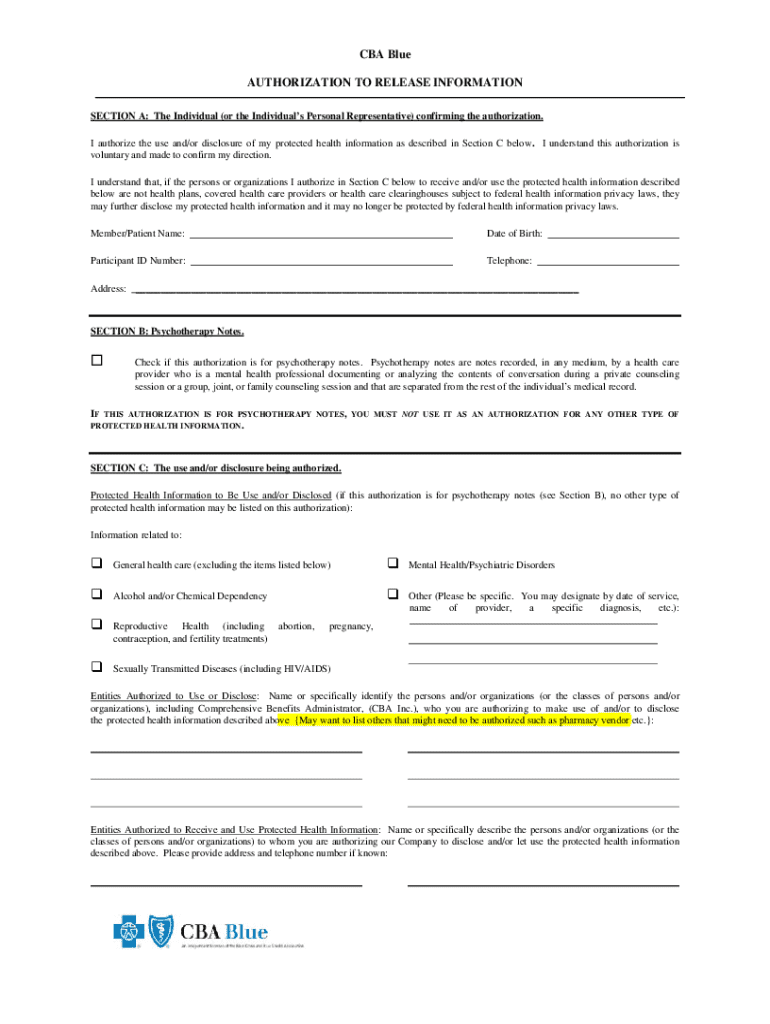
Get the free Cba Blue Authorization to Release Information
Get, Create, Make and Sign cba blue authorization to
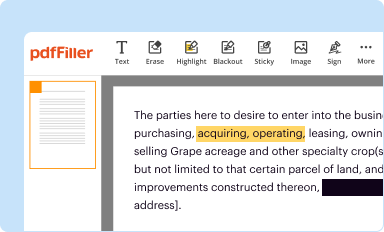
How to edit cba blue authorization to online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cba blue authorization to
How to fill out cba blue authorization to
Who needs cba blue authorization to?
CBA Blue Authorization to Form: A Comprehensive How-to Guide
Understanding CBA Blue Authorization
CBA Blue Authorization is an essential process within the realm of health insurance, specifically concerning the approval mechanisms utilized by providers and patients to secure necessary medical services. This authorization ensures that the health services proposed are covered under the insurance policy, aiding in streamlined patient care. The CBA Blue Authorization process safeguards both patients’ interests, by ensuring they receive medically necessary treatments, and payers’ interests, by preventing unnecessary expenditures.
In today's healthcare landscape, obtaining authorization is a pivotal step. The importance of CBA Blue Authorization extends beyond mere compliance; it acts as a critical checkpoint to ensure alignment of proposed treatments with established medical guidelines and policies. For both health providers and patients, an understanding of the CBA Blue Authorization process is crucial for effective navigation of insurance requirements.
Who needs to request authorization?
Typically, authorization requests must be submitted by either healthcare providers or patients, contingent upon the specific insurance plan requirements. Generally, this includes cases where certain treatments, procedures, or specialist visits may require prior approval. Eligible candidates for authorization requests encompass a variety of individuals, including those undergoing extensive medical procedures, patients requiring high-cost medications, and individuals seeking specialist consultations that exceed routine care.
Common scenarios necessitating the need for authorization include surgeries, advanced imaging procedures like MRIs, and referrals for specialized medical care. Understanding who needs to initiate a request allows for proactive management of healthcare services, ultimately leading to expedited care delivery.
Overview of the CBA Blue Authorization process
Navigating the CBA Blue Authorization process can seem daunting at first, but breaking it down into clear, actionable steps can make it much more manageable. Here is a practical step-by-step guide to initiating and following through the authorization process.
By following these structured steps, both patients and healthcare providers can significantly enhance the likelihood of securing the necessary authorization swiftly and with minimal delays.
Resources for CBA Blue Authorization
For individuals navigating the CBA Blue Authorization, various resources can simplify the experience. One effective resource is the interactive tools available on platforms that support document management, like pdfFiller. These tools make it easier to find and navigate online forms and check the status of authorization requests.
Frequently asked questions (FAQs) also represent an invaluable resource, addressing common concerns that arise during the authorization process. Some crucial questions include:
Special considerations for providers
Healthcare providers play a crucial role in the CBA Blue Authorization process. When submitting an authorization request on behalf of a patient, it’s vital to include all necessary details that clearly communicate the rationale for treatment. This includes not just the patient’s information but also comprehensive clinical documentation that justifies the service's medical necessity.
Additionally, providers must adhere to clear communication protocols with the insurer. Timely and thorough communication can often bridge gaps that lead to authorization delays. Common challenges faced by providers include incomplete information requests from insurers and unforeseen delays in authorization responses, both of which can be mitigated through diligent follow-up and proactive documentation.
Additional forms related to CBA Blue Authorization
In addition to the primary authorization form, there are a variety of prior approval forms that may be required during the CBA Blue Authorization process. These encompass any additional documentation that supports the medical necessity of the treatment, ensuring that all bases are covered before submission.
Providers are also advised to keep track of their provider change forms and related resources. Engaging with tools that simplify the updating of provider information in the authorization database can streamline the process and prevent potential search and retrieval issues during subsequent requests.
Frequently encountered issues
While navigating the CBA Blue Authorization process, various common challenges can arise, including problems with online submissions and delays that stem from missing documentation. It is essential to establish a systematic approach to avoid these pitfalls.
Implementing best practices in submissions can significantly improve the overall process. Tips for successful authorizations include ensuring thorough and complete submissions and maintaining timely follow-ups with insurers for progress updates.
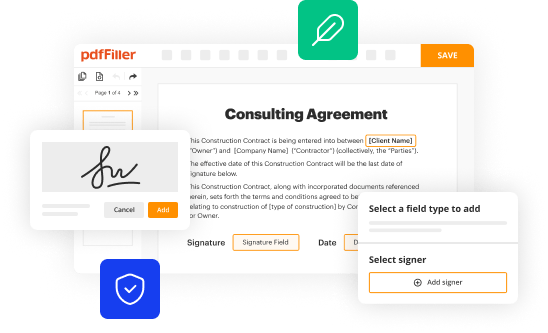
Interactive and collaborative features on pdfFiller
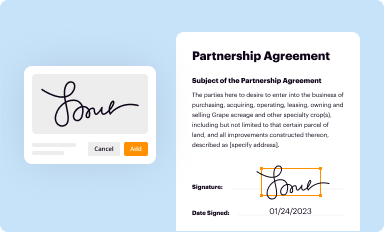
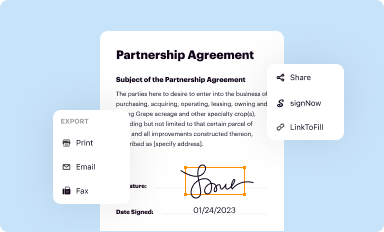
Utilizing tools like pdfFiller can immensely ease the process of handling CBA Blue Authorization documents. The platform supports seamless editing of PDF forms, allowing users to make necessary changes quickly and effectively. Moreover, eSigning capabilities streamline the signing process, enhancing efficiency.
Collaboration tools offered by pdfFiller facilitate teamwork among healthcare teams. Documents can be shared and managed between team members, contributing to real-time updates and notifications about document statuses. This collaborative feature is critical in ensuring that all information is up-to-date and accessible, which is especially vital during urgent authorization requests.
Knowledge base and community support
For those seeking assistance with the CBA Blue Authorization process, reaching out to customer service representatives can provide personalized help. Additionally, community forums are valuable for sharing experiences and advice, allowing individuals and teams to support each other through the complexities of authorization.
Staying informed on policy changes is vital for continued success in managing authorization requests. Engaging with newsletters or alerts from platforms like pdfFiller can help users keep up with the latest updates and guidelines related to CBA Blue Authorization, ensuring preparedness for any changes that may arise.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit cba blue authorization to straight from my smartphone?
How do I complete cba blue authorization to on an iOS device?
How do I complete cba blue authorization to on an Android device?
What is cba blue authorization to?
Who is required to file cba blue authorization to?
How to fill out cba blue authorization to?
What is the purpose of cba blue authorization to?
What information must be reported on cba blue authorization to?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.