Get the free Caremark Speciality Pharmacy Prior Authorization Forms
Get, Create, Make and Sign caremark speciality pharmacy prior
How to edit caremark speciality pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out caremark speciality pharmacy prior
How to fill out caremark speciality pharmacy prior
Who needs caremark speciality pharmacy prior?
Navigating the Caremark Specialty Pharmacy Prior Form: A Comprehensive Guide
Understanding the Caremark Specialty Pharmacy Prior Form
Prior authorization (PA) is a key process in the healthcare system designed to determine whether a specific prescription medication will be covered by insurance before it is dispensed. For patients using specialty medications, which often come with a higher cost and complex treatment protocols, the PA process is particularly important. The Caremark Specialty Pharmacy Prior Form is a tool that facilitates this process, ensuring that essential treatments can be accessed by patients who truly need them.
Caremark plays a critical role in managing prior authorizations, acting as an intermediary between patients, healthcare providers, and insurance companies. By filling out the Caremark Specialty Pharmacy Prior Form, healthcare providers can submit necessary documentation that supports the medical necessity of a requested specialty medication.
Prerequisites for using the Caremark Specialty Pharmacy Prior Form
Before diving into the form, there are a few prerequisites that must be met to ensure successful processing. Firstly, eligibility requirements must be confirmed, beginning with gathering detailed patient information. This includes full name, date of birth, and relevant contact information.
In addition, certain documentation is required alongside the form, including insurance information, which proves that the patient's plan provides coverage for the requested medication, and a medical history that supports the need for the medication.
Step-by-step instructions for completing the Caremark Specialty Pharmacy Prior Form
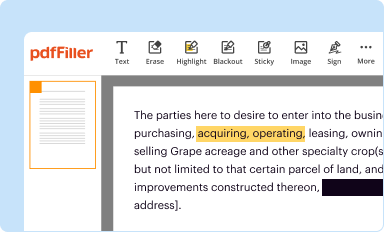
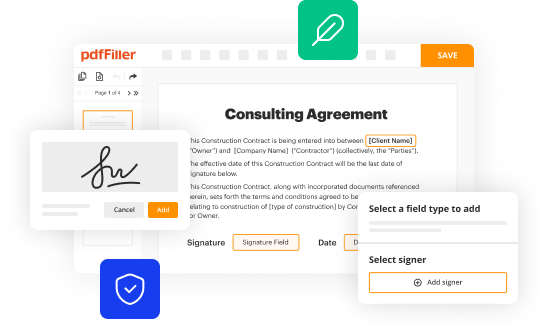
Completing the Caremark Specialty Pharmacy Prior Form can be done smoothly by following a series of straightforward steps. The first step is accessing the form, which is available on platforms like pdfFiller. You can navigate directly to the Caremark form section, where the form is hosted for easy access.
Next, begin filling out the form. Each section asks for specific details, including patient information, provider information, medication and dosage details, and an explanation of medical necessity.
pdfFiller also offers editing functionalities, which can enhance the accuracy of the information entered. Utilize these tools to ensure all fields are filled out correctly.
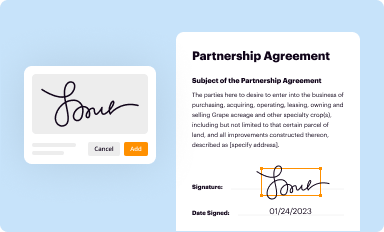
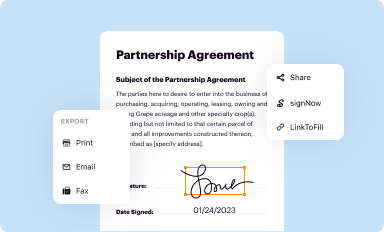
Once completed, eSignature tools available on pdfFiller allow users to sign the document digitally, simplifying the submission process and ensuring quick processing times.
Submission process for the Caremark Specialty Pharmacy Prior Form
After filling out the Caremark Specialty Pharmacy Prior Form, the next step is submission. With the pdfFiller platform, digital submission can be completed effortlessly. Simply follow these steps to send the form to Caremark.
Once submitted, it’s important to verify the status of your application through the pdfFiller platform. Watch out for common mistakes that can halt the process; thus, a checklist can be beneficial.
After submission: what to expect
Following the submission of the Caremark Specialty Pharmacy Prior Form, it's essential to understand the review process that follows. Caremark assesses the forms based on specific criteria, and the timeline for approval can vary.
Communication from Caremark will inform you about the status of your prior authorization request. Familiarize yourself with the types of notifications you may receive, and prepare for the next steps depending on the approval status.
Troubleshooting common issues
If your request is denied, understanding the reasoning is pivotal. Common denial reasons can include insufficient medical justification or lack of coverage under the patient's health plan.
In addition to appeals, you may encounter technical issues while submitting the form. pdfFiller provides support resources that can be invaluable for troubleshooting these problems quickly and efficiently.
Frequently asked questions (FAQs) about the Caremark Specialty Pharmacy Prior Form
To assist users in navigating the Caremark Specialty Pharmacy Prior Form, here are some frequently asked questions that address common concerns and queries.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out caremark speciality pharmacy prior using my mobile device?
Can I edit caremark speciality pharmacy prior on an Android device?
How do I fill out caremark speciality pharmacy prior on an Android device?
What is caremark speciality pharmacy prior?
Who is required to file caremark speciality pharmacy prior?
How to fill out caremark speciality pharmacy prior?
What is the purpose of caremark speciality pharmacy prior?
What information must be reported on caremark speciality pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.