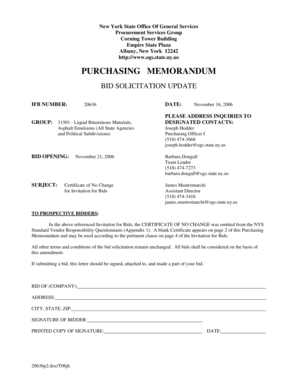
Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form



Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form

How to fill out prior authorization request form
Who needs prior authorization request form?
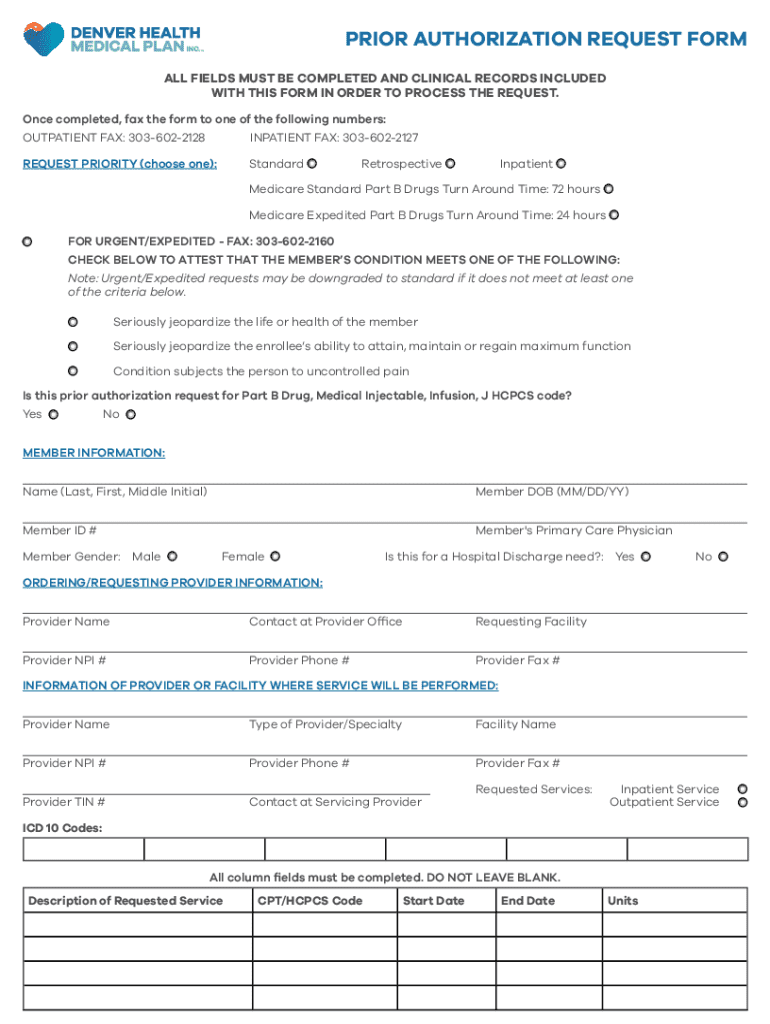
Understanding the Prior Authorization Request Form: A Complete Guide
Understanding prior authorization
Prior authorization is a process used by health insurance companies to determine if they will cover a prescribed treatment, service, or medication. By requiring healthcare providers to obtain approval before proceeding, insurers aim to manage costs and ensure that requested services meet their guidelines for medical necessity.
The importance of prior authorization in healthcare cannot be overstated. It helps prevent unnecessary treatments, ensures that patients receive the most appropriate care, and allows insurance companies to manage their expenditures effectively. Certain scenarios, such as surgeries, advanced imaging services like MRIs, or high-cost medications, frequently require prior authorization.
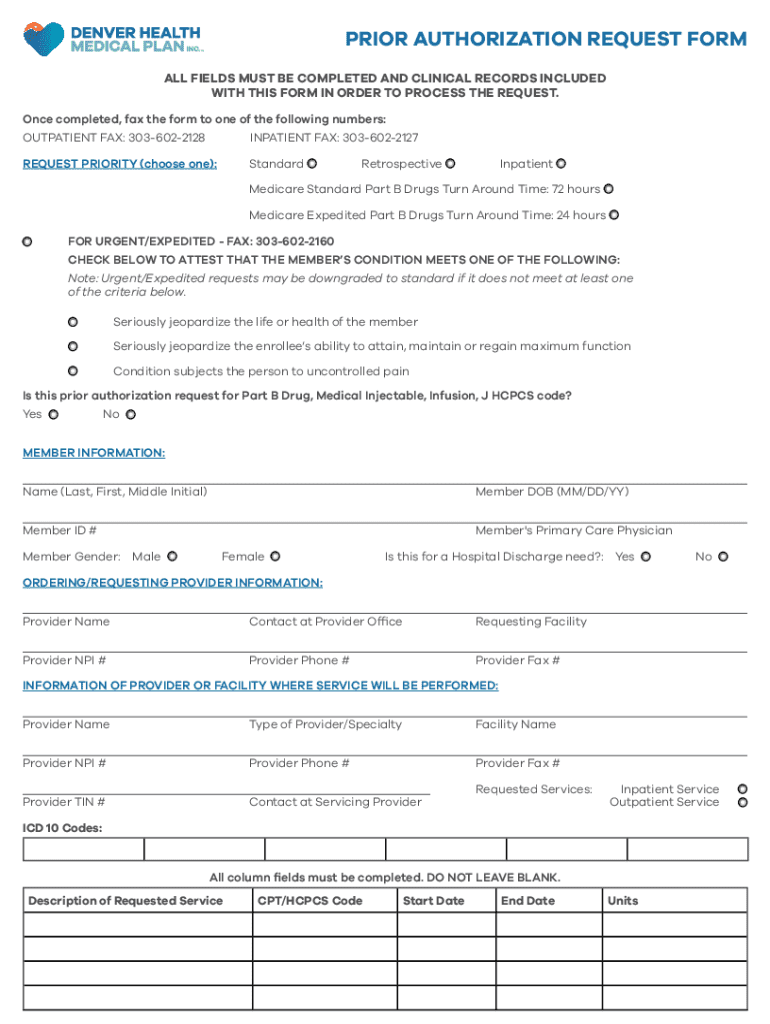
Overview of the prior authorization request form
A prior authorization request form is the official document submitted to an insurance provider, requesting approval for a specific treatment or service. It serves as a formal communication channel between healthcare providers and insurers, detailing essential information needed to assess the request.
Key components of the prior authorization request form typically include several crucial sections:
How to complete a prior authorization request form
Completing a prior authorization request form accurately is essential for timely approval. Here’s a step-by-step guide to navigating the process.
Editing and customizing the form with pdfFiller
pdfFiller offers robust tools for modifying your prior authorization request form. Users can not only fill out the form but can also make necessary edits to accommodate specific requirements.
With pdfFiller, you can utilize features that enable you to add, remove, or edit fields easily, streamlining the process. Collaborating with team members is also simple, ensuring everyone involved can contribute to the request efficiently.
Submitting the prior authorization request
Once the prior authorization request form is completed, submission is the next critical step. There are various methods available to submit the request, depending on the insurance provider’s preferences.
Tracking submission status is crucial; many insurance companies provide online tracking options. If your request is denied, understanding the reason behind the denial and gathering necessary evidence can help in re-submitting a strengthened request.
Managing your prior authorization requests
Management of prior authorization requests is key to ensuring an efficient workflow. Utilizing pdfFiller’s features can help you organize submitted requests and streamline the overall process.
Creating templates for future requests saves time and ensures consistency across submissions. Keeping track of approval and denial dates helps in addressing follow-ups and managing patient care more effectively, providing patients with timely responses.
Frequently asked questions (FAQs)
Understanding common questions related to the prior authorization process can demystify the experience for both providers and patients. Some inquiries that frequently arise include the necessity of authorization for different services, what to do if a request is denied, and communication tips with insurers.
Best practices for successful prior authorization requests
To increase the likelihood of approval for your prior authorization requests, consider adopting these best practices.
Utilizing pdfFiller for ongoing document management
pdfFiller’s cloud-based platform offers numerous advantages, especially in managing your prior authorization documents. The robust features allow for easy access and collaboration, regardless of location.
Accessibility features are particularly beneficial for teams, enabling multiple users to edit, review, and approve documents instantly. Secure storage and sharing options also ensure that sensitive patient information remains protected while being readily available when needed.
Interactive tools & resources within pdfFiller
pdfFiller provides a suite of customizable tools and resources that enhance your experience with prior authorization requests. Users can access form templates that fit their needs, ensuring accuracy and compliance.
Additionally, helpful guides and articles are available to educate users on best practices and potential pitfalls, while support resources provide assistance whenever needed, ensuring a smooth user experience.
Enhancing workflow with pdfFiller
Integrating prior authorization requests into daily operations can be challenging. However, using pdfFiller’s platform enables seamless incorporation of these requests into your workflow.
The ability to collaborate using editing and eSigning features helps streamline communication among team members. Adopting such tools can improve efficiency and ensure that every team member is aware of the current status of requests.
Real-life case studies
Practical examples of teams successfully utilizing pdfFiller for prior authorization can shed light on its efficacy. These success stories highlight the enhanced productivity achieved by streamlined document management and collaboration features.
Many healthcare teams have reported a significant reduction in the time taken to complete prior authorization requests, leading to improved patient care and quicker response times. These case studies serve to validate the positive impact of leveraging technology in healthcare document processes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get prior authorization request form?
How do I edit prior authorization request form in Chrome?
How do I fill out prior authorization request form using my mobile device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.