Get the free Tepezza Pharmacy Prior Authorization Request Form
Get, Create, Make and Sign tepezza pharmacy prior authorization
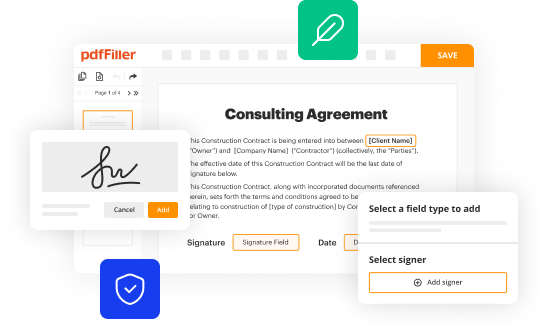
How to edit tepezza pharmacy prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out tepezza pharmacy prior authorization
How to fill out tepezza pharmacy prior authorization
Who needs tepezza pharmacy prior authorization?
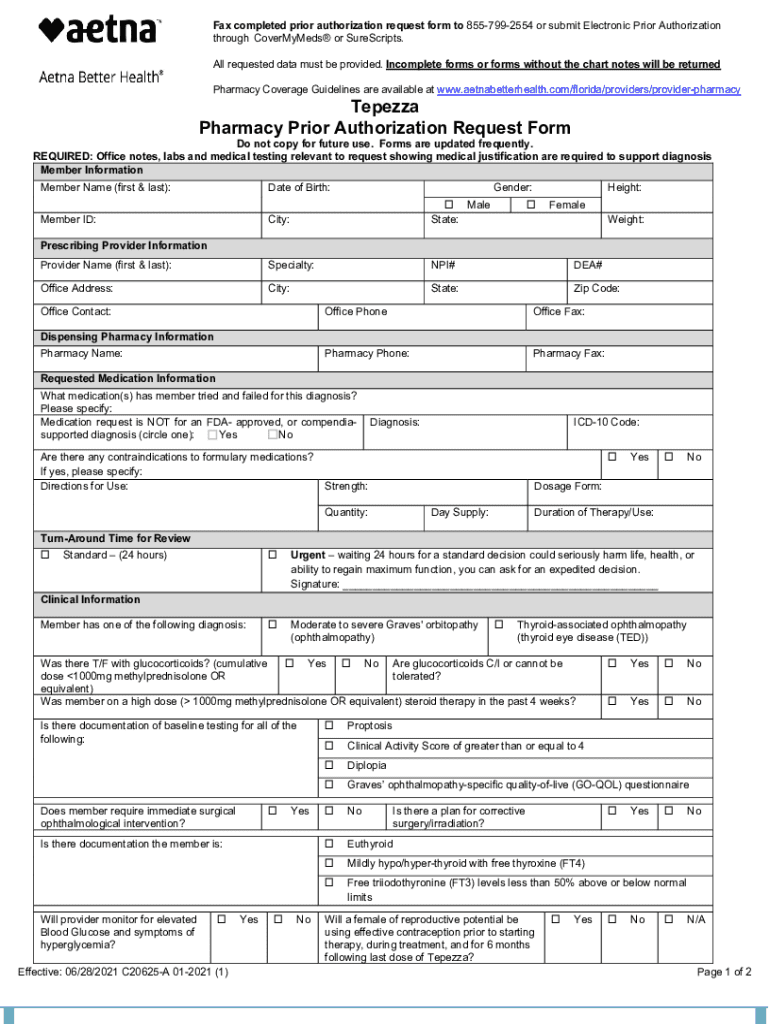
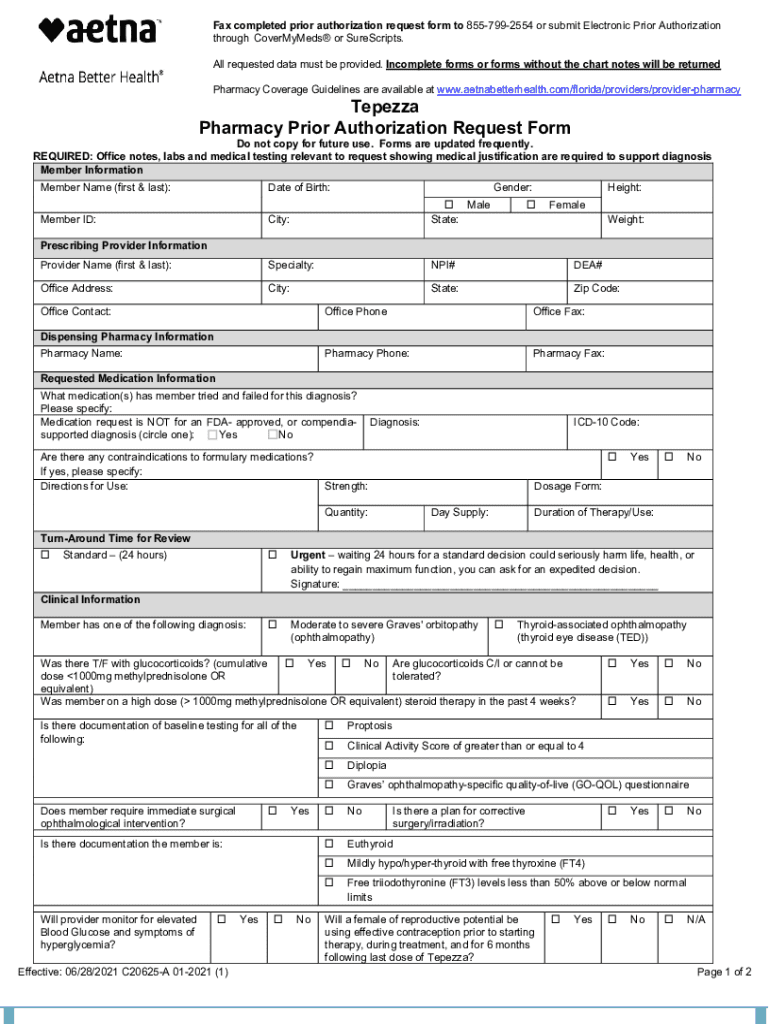
Understanding the Tepezza Pharmacy Prior Authorization Form
Understanding the Tepezza prior authorization process
Tepezza, the first FDA-approved treatment for thyroid eye disease, offers hope to patients suffering from this condition. It is crucial for patients to understand that while Tepezza can significantly improve symptoms like bulging eyes and double vision, obtaining it is not as straightforward as a regular prescription. The Tepezza pharmacy prior authorization form plays a vital role in the accessibility of this medication.
Prior authorization is required by many insurance companies to ensure that the treatment is both necessary and appropriate for the patient’s condition. This step is essential in the healthcare management process, acting as a safeguard to confirm that patients receive targeted treatments suited for their medical needs. It protects insurers from covering medications that may not be effective for certain patients or conditions.
Preparing to fill out the Tepezza pharmacy prior authorization form
Before starting to fill out the Tepezza pharmacy prior authorization form, it's crucial to ensure that the patient meets specific eligibility criteria. Generally, Tepezza is prescribed for patients diagnosed with moderate to severe thyroid eye disease who have not adequately responded to prior treatments. Healthcare providers should conduct a thorough assessment, which may include imaging tests and clinical evaluations, to confirm eligibility.
Additionally, specific documentation is required for the submission of the prior authorization form. This includes comprehensive patient demographic details, insurance information, and a medical history that outlines the patient’s previous treatments and responses to therapies. Accurate and detailed information not only facilitates the approval process but also avoids unnecessary back-and-forth with the insurance provider.
Step-by-step guide to completing the Tepezza prior authorization form
Filling out the Tepezza pharmacy prior authorization form can feel complex, but breaking it down into manageable sections can simplify the process. The first section typically captures patient information, which must include the patient's name, date of birth, and contact details. It's crucial to ensure that all details are entered accurately to prevent delays.
The next section focuses on treatment information. Here, you must list the prescribed dosage and frequency of Tepezza. It's beneficial to also document prior treatments and responses in this section. This information strengthens the justification for the prescribed medication and clearly articulates the treatment journey.
Further into the form, you’ll encounter a section dedicated to medical necessity. This part often requires supporting documentation such as letters of medical necessity and clinical notes from healthcare providers that outline the rationale for prescribing Tepezza. Such documents play a critical role in substantiating the request and aiding in a favorable evaluation by the insurer.
Lastly, the insurance and billing details section is crucial. Here, accurately entering the patient's insurance information is vital. Be aware of common pitfalls, such as omitting policy numbers or providing incorrect insurance provider details, as these can lead to delays or rejections.
Submitting the Tepezza prior authorization form
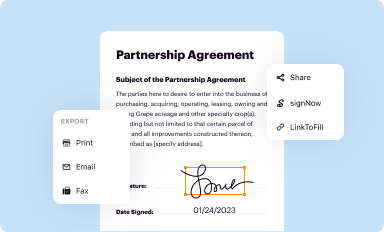
Once the Tepezza pharmacy prior authorization form is completed, submission options vary based on the insurance provider's preferences. Many insurers facilitate electronic submission, which can expedite the approval process. Ensure that you follow best practices for electronic submissions, like confirming receipt and keeping a copy of the submitted documents.
For those opting for paper submissions, it’s advisable to send the form via certified mail. After submission, follow-up is key; periodically check the status to anticipate approval or further actions needed. Understanding typical timelines for approval can help manage patient expectations, as responses can range from a few days to several weeks.
Resources for managing denials and appeals
Despite careful preparation, denials of the Tepezza pharmacy prior authorization request can occur. It's essential to be aware of common reasons for denial, such as insufficient documentation, lack of medical necessity, or not meeting specific insurance criteria. Understanding these can help you anticipate what may need to be addressed in an appeal.
If a denial occurs, appealing it is crucial. Key elements of a strong appeal letter include a clear expression of the reasons for the denial, supporting evidence from medical professionals, and detailed information about the patient’s needs. Important documentation, such as letters from healthcare providers and patient records, should accompany the appeal to strengthen the case.
For those seeking guidance in writing appeal letters, templates can provide a helpful framework. A standard letter of medical necessity template and a payor appeal letter template can help streamline the process, ensuring that all necessary points are covered and properly formatted.
Additional support resources
Patients navigating Tepezza treatment can find educational resources valuable. Infographics and literature detailing the treatment process and what to expect can significantly reduce anxiety. Furthermore, guides for the infusion experience can prepare patients for what they’ll encounter during treatment.
Practitioners can also benefit from tools such as clinical documentation guides and billing and coding guides specific to Tepezza. These resources can help streamline clinical admin processes and improve accuracy in paperwork. Additionally, compiling a list of frequently asked questions regarding Tepezza and the prior authorization process can serve as a quick reference for both patients and providers.
Conclusion and next steps
Organizing documentation is crucial during the Tepezza prior authorization process. Keep track of all submitted forms and correspondence with insurers. Quick tips for future prior authorization submissions include double-checking all entries for accuracy, having a checklist of required documents, and understanding your insurance provider's specific submission guidelines.
By following these steps and utilizing available resources, you can navigate the Tepezza pharmacy prior authorization form process with confidence, ensuring that needed treatment is accessed in a timely manner.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my tepezza pharmacy prior authorization directly from Gmail?
Can I create an eSignature for the tepezza pharmacy prior authorization in Gmail?
How do I complete tepezza pharmacy prior authorization on an iOS device?
What is tepezza pharmacy prior authorization?
Who is required to file tepezza pharmacy prior authorization?
How to fill out tepezza pharmacy prior authorization?
What is the purpose of tepezza pharmacy prior authorization?
What information must be reported on tepezza pharmacy prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.