Get the free Request for Prior Authorization
Get, Create, Make and Sign request for prior authorization



How to edit request for prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out request for prior authorization

How to fill out request for prior authorization
Who needs request for prior authorization?
Request for Prior Authorization Form: A Comprehensive How-to Guide
Understanding prior authorization
Prior authorization is a critical component within the healthcare system that ensures certain medical services, treatments, or medications are deemed necessary by a patient's insurance provider before they are approved for coverage. This step not only checks the appropriateness and necessity of the proposed healthcare action but also helps manage costs for both patients and insurers. The requirement for prior authorization has increased over recent years as insurance companies seek to control spending.
The importance of prior authorization cannot be understated, as it acts as a gatekeeping mechanism that protects patients from unnecessary or ineffective procedures while ensuring that providers operate within the financial frameworks set by insurance companies. Furthermore, prior authorizations can prevent future disputes regarding coverage and payments by clarifying service expectations upfront.
The significance of the request for prior authorization form
Utilizing the request for prior authorization form streamlines the entire approval process. By providing standardized information and documentation, healthcare providers can effectively communicate the medical necessity of a service or treatment to the insurer. This helps reduce unnecessary delays in patient care, often resulting in better health outcomes.
This form is crucial not only for healthcare providers seeking timely approvals but also for patients who may wish to understand more about their coverage options and the steps associated with obtaining necessary care. Administrative teams within healthcare facilities also benefit from utilizing the form to streamline workflows, track requests, and handle communications with insurers.
Accessing the request for prior authorization form
Finding the request for prior authorization form is straightforward with pdfFiller. Users can navigate through the platform’s interface to access a variety of forms relevant to their needs. Simply search for 'prior authorization form' in the search bar, and you will be presented with a list of templates tailored to specific insurance providers.
In addition, pdfFiller supports individual customization, allowing users to fill out forms aligned with the specific requirements of different insurers. This feature is essential since various insurance companies may have specific forms they accept for their prior authorization requests.
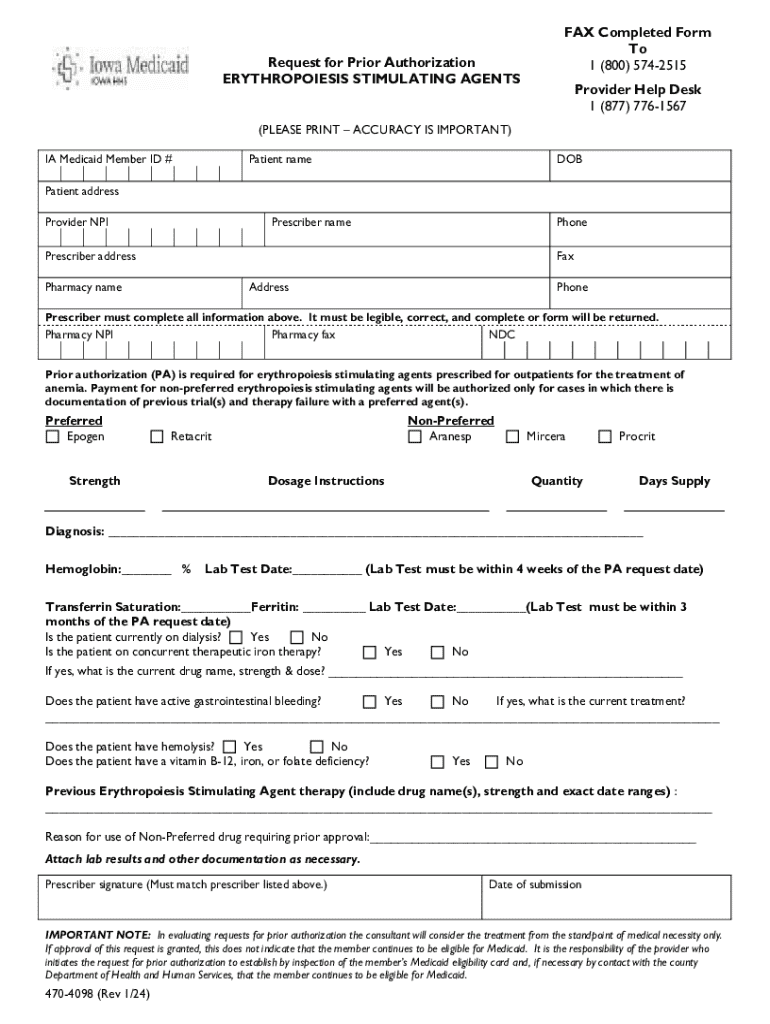
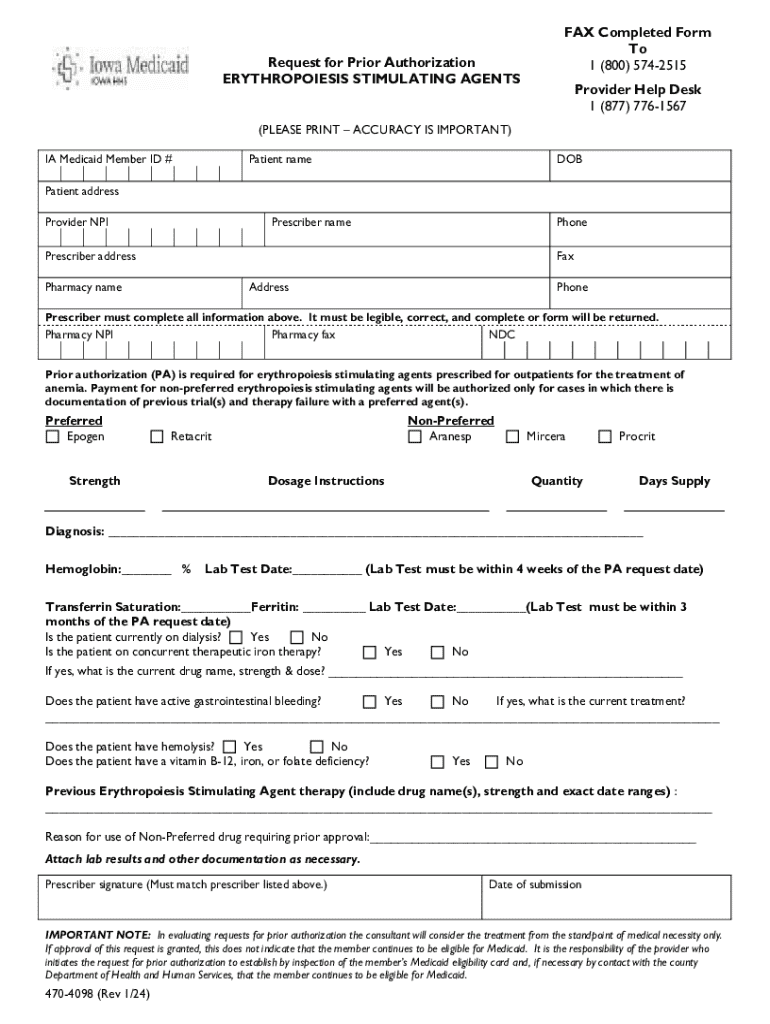
Completing the request for prior authorization form
Completing the request for prior authorization form is a methodical process. Start by gathering essential information about the patient. This includes personal identification information, date of birth, and insurance details, as well as the provider's information such as name, practice address, and contact number.
Once gathered, the next step involves filling out the form correctly. Ensure that you accurately record the procedure or service being requested, providing any necessary clinical information that justifies the request. It's crucial to double-check for any mistakes to prevent delays in processing.
After filling out the form, reviewing your submission is vital. Ensure all areas are correctly completed and check for any missing documentation. Accurate information not only facilitates the approval process but also minimizes chances of denial.
pdfFiller provides interactive tools to assist in form completion. Features such as electronic signatures, real-time collaboration, and editing capabilities available on the platform enhance the overall experience and help ensure that the form is accurately filled out.
Submitting the form
Once the request for prior authorization form is completed, the method of submission can greatly affect how quickly your request is processed. pdfFiller offers various online submission options, which tend to be faster. Utilize the built-in submission feature to directly send the completed form to your insurer.
Emailing or mailing the form are other options, although each comes with pros and cons. Emailing is typically quicker but can be prone to delivery and spam issues, while mailing provides a physical record but takes longer. Consider your options carefully to ensure timely submission.
Tracking your submission is crucial. With pdfFiller, users can easily monitor the status of their request, which allows proactive follow-ups if the submission remains unacknowledged for an extended period.
Post-submission considerations
After submitting your request for prior authorization, it is essential to understand what happens next. Each insurer has their own timelines for reviewing submissions, which can often range from a few days to a few weeks. During this period, the insurance company may reach out for further information or clarification regarding the request.
In the case of a denial, knowing how to proceed is critical. Common reasons for denials include missing information, failure to meet medical necessity criteria, or the procedure being deemed experimental. If the authorization is not granted, patients and providers can initiate an appeal, which typically involves providing additional documentation to support the request.
Best practices for requesting prior authorizations
Adopting best practices when requesting prior authorizations can save time and reduce frustration. Familiarize yourself with specific insurance protocols, as many companies offer resources such as webinars and guides tailored to navigating their specific processes.
Using pdfFiller effectively empowers users to manage documentation seamlessly, from creating and editing forms to collaborating and storing information securely in the cloud. This capability is particularly valuable for healthcare teams that need to handle multiple requests concurrently.
Frequently asked questions (FAQs)
You may have questions about the request for prior authorization form, especially regarding incomplete information or submission protocols. Here are some frequently asked questions that can guide you through the process.
User testimonials and success stories
Real-life experiences using the request for prior authorization form can illustrate its efficacy in the healthcare process. Users often share positive feedback regarding how pdfFiller has streamlined their document management. Many have reported faster approvals due to accurate submissions and thorough tracking capabilities.
Healthcare providers frequently note that the ease of collaboration facilitated by pdfFiller has fostered better communication between patients and insurers, ultimately resulting in improved care experiences.
Advanced tools for document management
pdfFiller not only simplifies form creation but also integrates a suite of advanced tools designed to enhance document management efficiency. Features like eSigning allow for quick approvals, and collaborative editing enables teams to work together without the hassle of multiple versions.
Moreover, the platform provides cloud storage solutions ensuring that all documents are accessible from anywhere. This flexibility crucially supports healthcare providers who need immediate access to patient files and prior authorizations anytime and anywhere.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my request for prior authorization directly from Gmail?
How do I complete request for prior authorization on an iOS device?
Can I edit request for prior authorization on an Android device?
What is request for prior authorization?
Who is required to file request for prior authorization?
How to fill out request for prior authorization?
What is the purpose of request for prior authorization?
What information must be reported on request for prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.