Get the free Arikayce Prior Authorization Request Prescriber Fax Form
Get, Create, Make and Sign arikayce prior authorization request
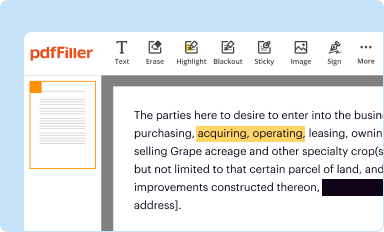
Editing arikayce prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out arikayce prior authorization request
How to fill out arikayce prior authorization request
Who needs arikayce prior authorization request?
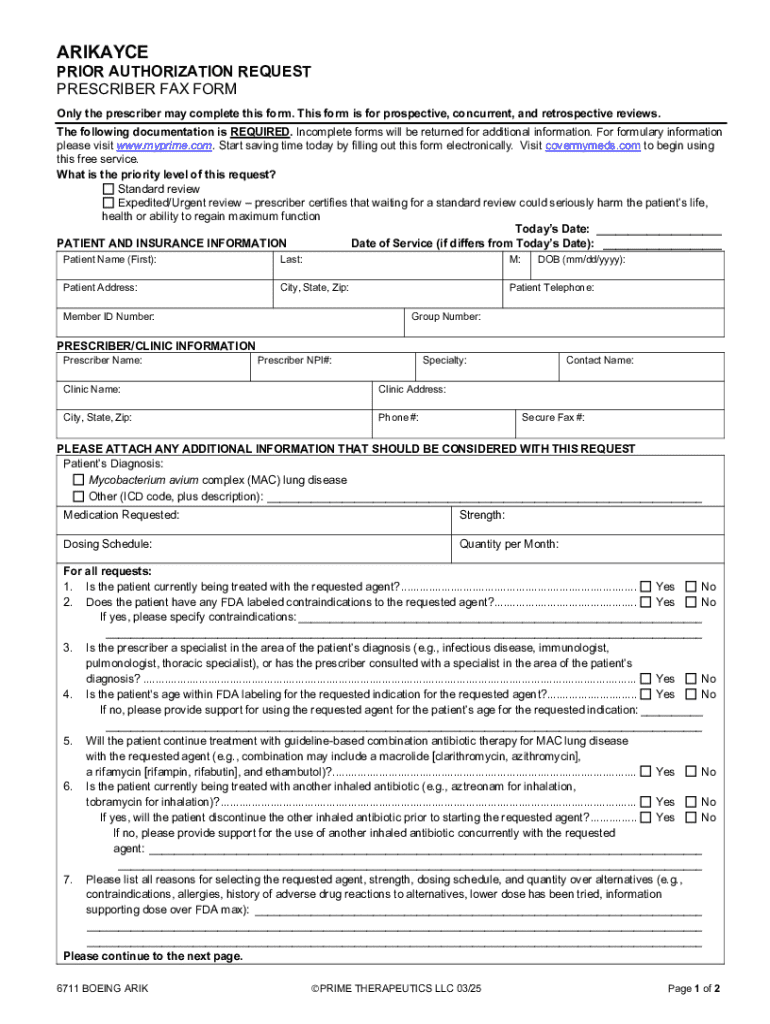
Arikayce Prior Authorization Request Form: Your Comprehensive Guide
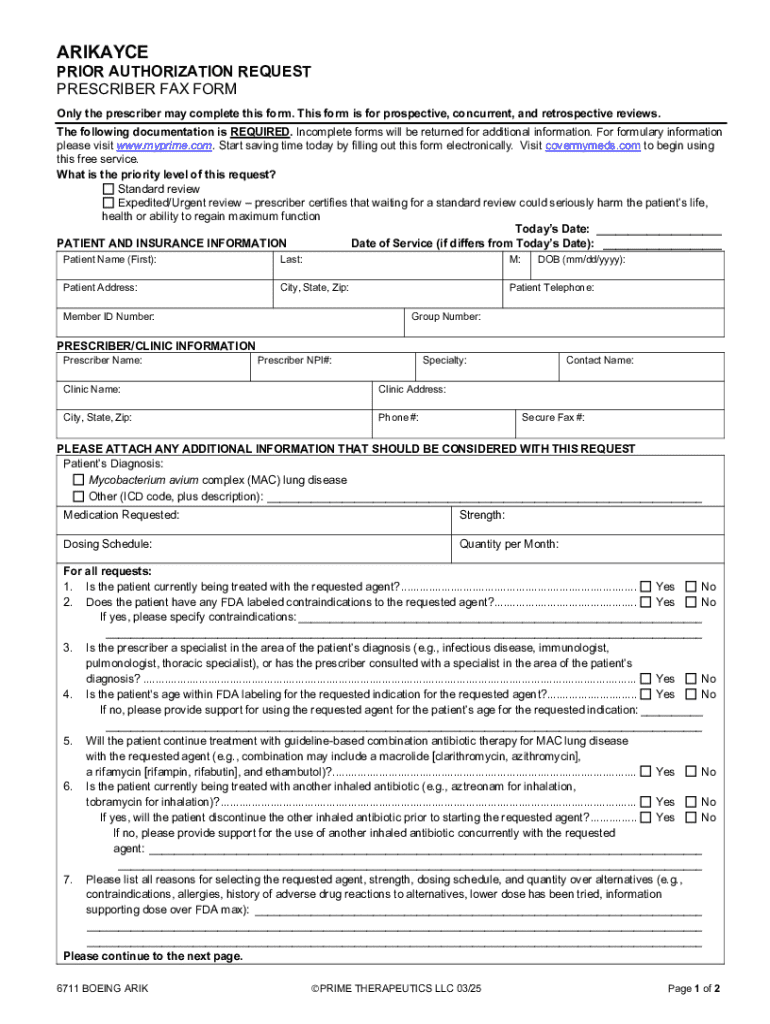
Understanding the Arikayce prior authorization process
Prior authorization is a crucial step needed before many insurance companies will cover certain medications and treatments, including Arikayce. It involves obtaining approval from the insurance provider to ensure that the prescribed medication is necessary for the patient’s health condition before the medication is dispensed or treatments are administered.
The importance of prior authorization for Arikayce cannot be understated. As a treatment specifically for lung infections caused by Mycobacterium avium complex (MAC) in patients with cystic fibrosis, it is critical to ensure that patients receive this specialized therapy without undue delays. Prior authorization helps to ensure that the patient truly meets the criteria set by the insurance provider for medication approval.
Key stakeholders in the process include:
Preparing your Arikayce prior authorization request
To initiate the prior authorization process for Arikayce, preparing a complete and accurate request is essential. Start by gathering necessary information, which includes patient information such as name, date of birth, and insurance details.
Next, ensure you include medication and dosage details. This includes the specific dosage of Arikayce prescribed and the frequency of administration. Additionally, a thorough medical history and diagnosis must be outlined, including the onset of the condition, previous treatments explored, and how they have contributed to the patient's healthcare journey.
Understanding the requirements established by your insurance company is equally vital. Each insurance provider may have specific policies related to Arikayce, so it’s important to review these requirements beforehand. Common reasons for denials often include insufficient documentation regarding medical necessity or failure to meet predetermined criteria.
Step-by-step guide to completing the Arikayce prior authorization request form
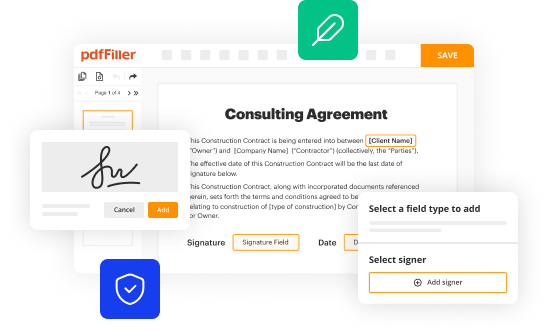
The process of completing the Arikayce prior authorization request form involves several key steps. First, accessing the form is straightforward. You can find the form online on the pdfFiller website. It can be easily downloaded and saved for your convenience.
Upon downloading, begin completing the form by accurately entering all patient information. Then, provide insurance information, which includes the policy number and any group numbers associated with the coverage. One of the most crucial components of the form is the medical necessity justification that must clearly explain why Arikayce is essential for the patient's treatment plan.
Additionally, be sure to add supporting documentation. This may include relevant medical records, previous treatment history, and provider notes that corroborate the necessity of Arikayce for the patient's health.
Submitting your prior authorization request
After assembling your Arikayce prior authorization request form and supporting documents, the next step is submission. Before sending it off, take a moment to review your completed form closely. Ensure that all required fields are filled accurately and that there are no errors that could lead to unnecessary delays.
Submission methods vary; they may include online submissions through your insurance provider's portal, faxing the request to the designated number, or mailing the form to the appropriate department. Always retain a copy of what you send for your own records.
Once submitted, it’s important to confirm that your request has been received. Tracking your request can be done through online systems where available, and understanding timeframes for approvals can help mitigate anxieties regarding the waiting period.
Navigating the response from insurance providers
Understanding the responses you receive from insurance providers, whether approval or denial, is critical to the process. Approval letters will typically include confirmation of coverage and any conditions that must be met during treatment. Denial letters will outline specific reasons for the unfavorable decision.
Common terms and phrases found in these letters often relate to medical necessity. If your request is denied, the first step is to assess why. This could involve reviewing the reasons stated in the denial letter. Many times, denial can be rebutted by providing additional documentation or clarification.
It’s advisable to engage with your healthcare provider to help navigate the appeals process. They can provide additional medical support and documentation which may be essential in overturning the denial decision.
Tips for a smooth Arikayce authorization experience
Effective communication with your healthcare provider is paramount for a successful prior authorization process. Ensure that they understand the urgency of obtaining Arikayce and can provide the necessary documentation promptly.
Additionally, staying organized with all relevant documentation will help facilitate a smoother process. Keeping copies of all correspondence, forms, and submissions can assist in tracking your authorization journey.
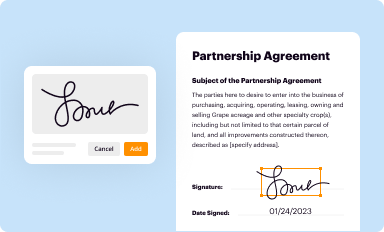
Utilizing tools like pdfFiller can also enhance your experience. Features such as editing and customizing the form can simplify preparation. E-signing documents provides a faster processing option, and collaborative features allow for team support, making it easier to gather input from multiple providers or team members involved in the patient's care.
Case studies: Successful prior authorization stories
Learning from patient experiences with Arikayce authorization can yield valuable insights. Many patients have encountered obstacles during the approval process, but those who remain diligent often find success. For instance, a patient who involved their healthcare provider early in the process, gathering extensive documentation and emphasizing the urgency of their medical condition, found success despite initial denials.
Lessons learned from such case studies include the importance of comprehensive documentation and proactive communication with insurance providers. Best practices highlight that patients who familiarize themselves with their insurance policies and stay persistent are more likely to succeed.
Frequently asked questions (FAQs)
A pivotal question many patients ask is, 'What is Arikayce?' Arikayce is an important inhaled medication designed to treat lung infections caused by the mycobacterial infection in patients with specific conditions.
Another frequently asked concern revolves around timing: 'How long does the prior authorization process take?' While this varies by insurance provider, it may take anywhere from a few days to a couple of weeks. Patience is essential during this timeframe as it can be both anxiety-inducing and critical for treatment.
Finally, if your insurance does not cover Arikayce, it can be distressing. Understanding alternative financial assistance programs and exploring appeals are pivotal steps. Engaging your healthcare provider can significantly aid in navigating these complexities.
Conclusion: Empowering your journey with pdfFiller
The process of obtaining an Arikayce prior authorization request form doesn’t have to be overwhelming. By utilizing cloud-based tools like pdfFiller, you can manage your documentation seamlessly and efficiently. Leveraging its capabilities empowers users to edit, e-sign, collaborate, and handle documents from anywhere.
The user-friendly interface and robust features simplify the often-complicated authorization process, allowing patients and providers to concentrate on what truly matters: patient care.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send arikayce prior authorization request for eSignature?
How do I edit arikayce prior authorization request straight from my smartphone?
How do I fill out the arikayce prior authorization request form on my smartphone?
What is arikayce prior authorization request?
Who is required to file arikayce prior authorization request?
How to fill out arikayce prior authorization request?
What is the purpose of arikayce prior authorization request?
What information must be reported on arikayce prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.