Get the free Medical Specialty Drug Authorization Request Form
Get, Create, Make and Sign medical specialty drug authorization
How to edit medical specialty drug authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medical specialty drug authorization
How to fill out medical specialty drug authorization
Who needs medical specialty drug authorization?
A comprehensive guide to the medical specialty drug authorization form
Understanding medical specialty drug authorization
Medical specialty drugs are high-cost medications used to treat complex or chronic conditions such as cancer, multiple sclerosis, and rheumatoid arthritis. These medications require special handling, administration, or monitoring, which also contributes to their elevated costs. Given these factors, the healthcare system mandates a robust authorization process to ensure that these expensive therapies are utilized appropriately.
Authorization serves several critical functions in healthcare. It protects patients from receiving medications that may not be clinically appropriate and helps insurance companies manage the financial implications of expensive treatments. The authorization process typically involves healthcare providers submitting an authorization request to insurance companies before administering specialty drugs.
Understanding the nuances of the authorization process is essential for healthcare providers to navigate the complexities of medical specialty drug approvals effectively.
Types of medical specialty drug authorizations
There are several types of authorizations that healthcare providers may encounter when prescribing medical specialty drugs. The primary types include prior authorization, step therapy, and quantity limits.
Prior authorization
Prior authorization is a requirement from the insurance company that must be fulfilled before a provider can prescribe certain medications. This measure is designed to ensure that the prescribed therapy aligns with the patient's medical needs and that less costly alternatives have been considered.
Providers are notified when prior authorization is required, typically through the patient’s insurance plan. It's important to note that coverage levels can vary based on the drug and the specific insurance policy.
Step therapy
Step therapy is a cost-control strategy wherein patients must try a different, usually less expensive medication before their insurer approves coverage for the requested specialty drug. This approach aims to ensure that healthcare resources are utilized efficiently while maintaining patient safety.
Quantity limits
Quantity limits refer to restrictions placed on the number of units of a medication that can be dispensed within a specified timeframe. These limits help control overall healthcare costs and ensure that patients are receiving these medications within safe parameters.
The role of healthcare providers
Healthcare providers play a crucial role in the medical specialty drug authorization process. They are responsible for initiating and facilitating the authorization requests, navigating complicated insurance requirements, and ensuring that patients receive the care they need without unnecessary delays.
Generally, any licensed healthcare provider, such as physicians, nurse practitioners, or physician assistants, can request authorization for a specialty drug for their patients. Their key responsibilities include:
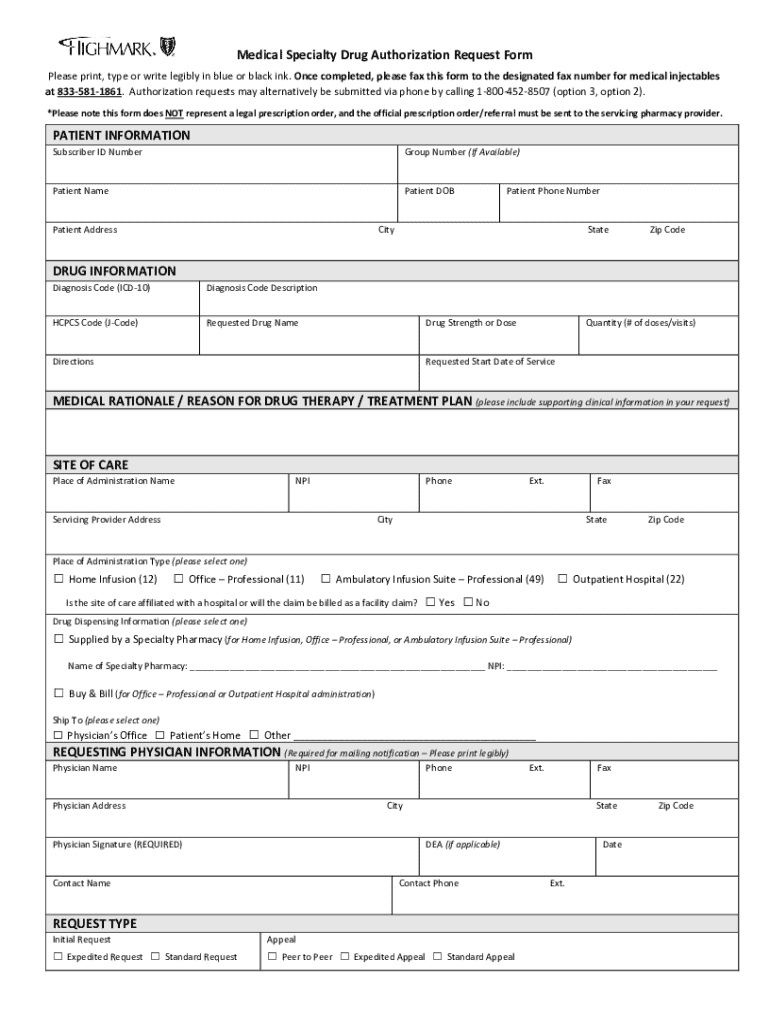
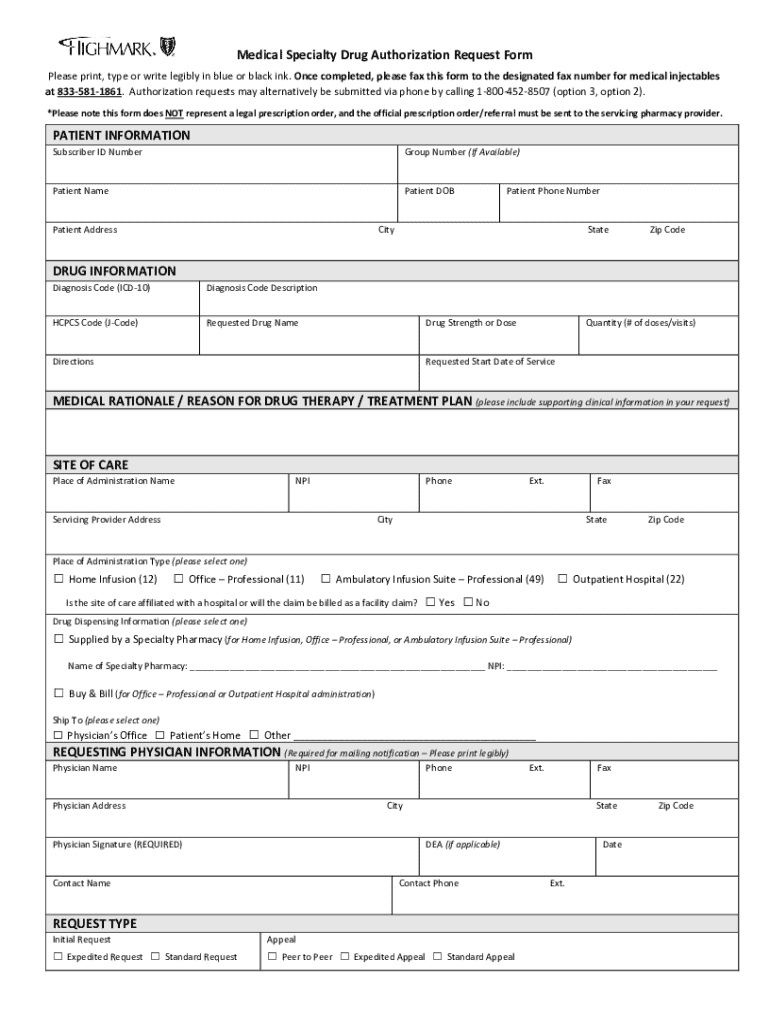
The authorization form: key components
Filling out the medical specialty drug authorization form correctly is vital for securing approval. The form typically includes several key sections that require detailed information to support the request.
Understanding the form essentials
Sections included in the form
Additionally, the form may require sections detailing the patient's diagnosis and medical history, along with a justification for the requested drug. This justification often includes clinical notes and relevant findings from the patient's medical records, aiming to demonstrate the necessity of the prescribed therapy.
Filling out the medical specialty drug authorization form
Completing the authorization form accurately is critical to avoiding delays or denials of critical medication. A step-by-step approach can simplify the process and ensure all required information is captured.
Common mistakes to avoid
Even minor errors in filling out the form can lead to significant delays. Some common pitfalls include:
Editing and customizing the authorization form
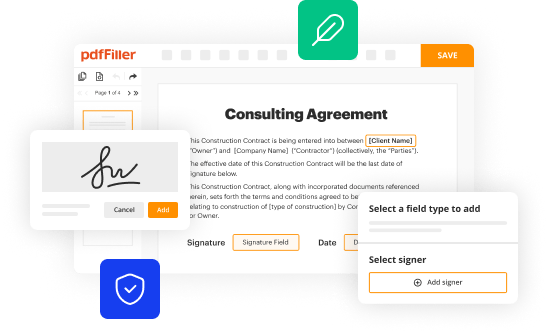
Using tools like pdfFiller can streamline the process of filling out and customizing the medical specialty drug authorization form. This platform allows for easy editing and uploading of necessary documents.
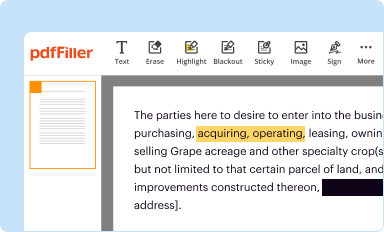
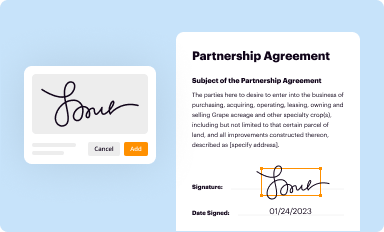
Using pdfFiller to edit your forms
The platform supports interactive tools that make the process efficient and user-friendly.
Utilizing interactive tools
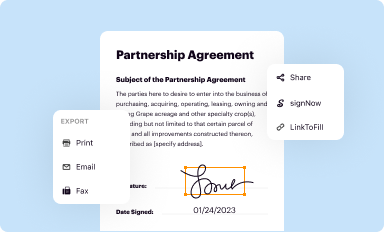
Submitting the authorization form
Once you have compiled and completed the medical specialty drug authorization form, the next crucial step is submission. Various methods exist for submitting these forms, each with unique advantages.
Essential steps for submission
Effective communication with insurance companies post-submission is essential for resolving issues and ensuring the authorization process flows smoothly.
Communication with insurance companies
Managing authorization status
After submission, it is essential to track the status of the authorization request to ensure it is being processed in a timely manner. Knowing how to manage authorization status effectively can help mitigate delays.
Dealing with denials
Denials of authorization requests can be frustrating, but understanding the common reasons for denial can help prepare for potential challenges.
Here are steps to take when a request is denied:
Best practices for authorization success
To facilitate a smoother authorization process, developing a systematic approach can be invaluable. Efficiency in managing authorization requests can save time for both providers and patients.
Leveraging technology for authorization management
Utilizing cloud-based solutions like pdfFiller can significantly enhance your ability to manage the authorization process efficiently. The advantages of using a centralized document management system simplify the entire workflow.
Preparing for future changes in authorization processes
The healthcare landscape is ever-evolving, and staying informed about policy changes regarding medical specialty drug authorization is crucial for providers.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an eSignature for the medical specialty drug authorization in Gmail?
How do I edit medical specialty drug authorization straight from my smartphone?
Can I edit medical specialty drug authorization on an Android device?
What is medical specialty drug authorization?
Who is required to file medical specialty drug authorization?
How to fill out medical specialty drug authorization?
What is the purpose of medical specialty drug authorization?
What information must be reported on medical specialty drug authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.