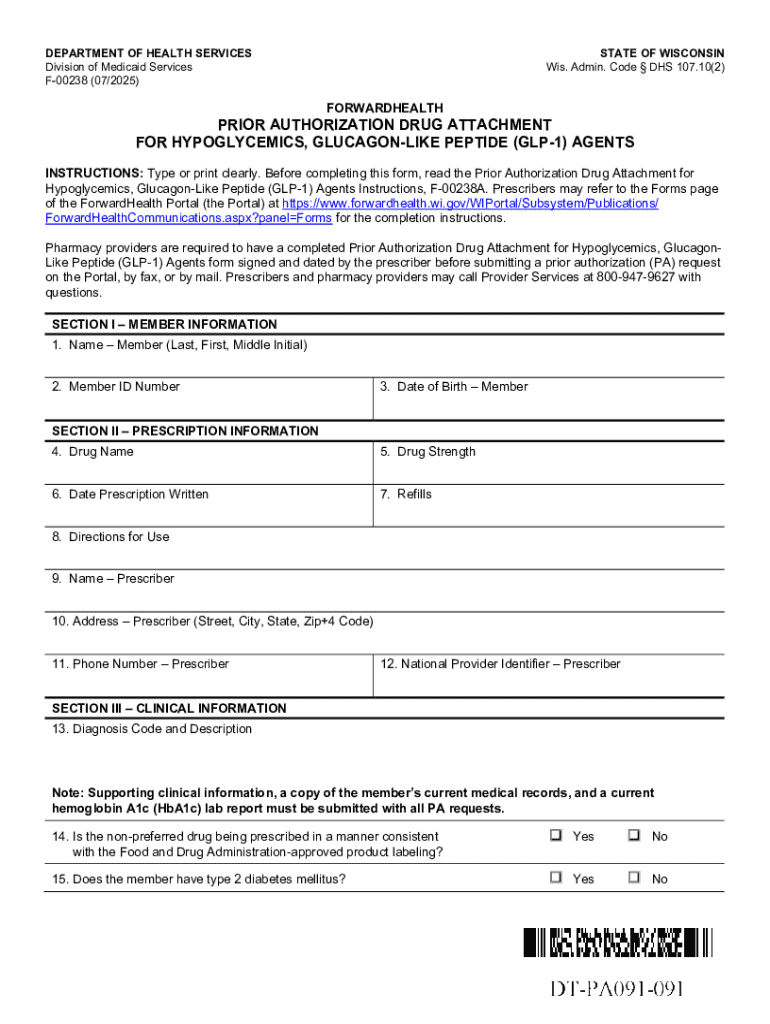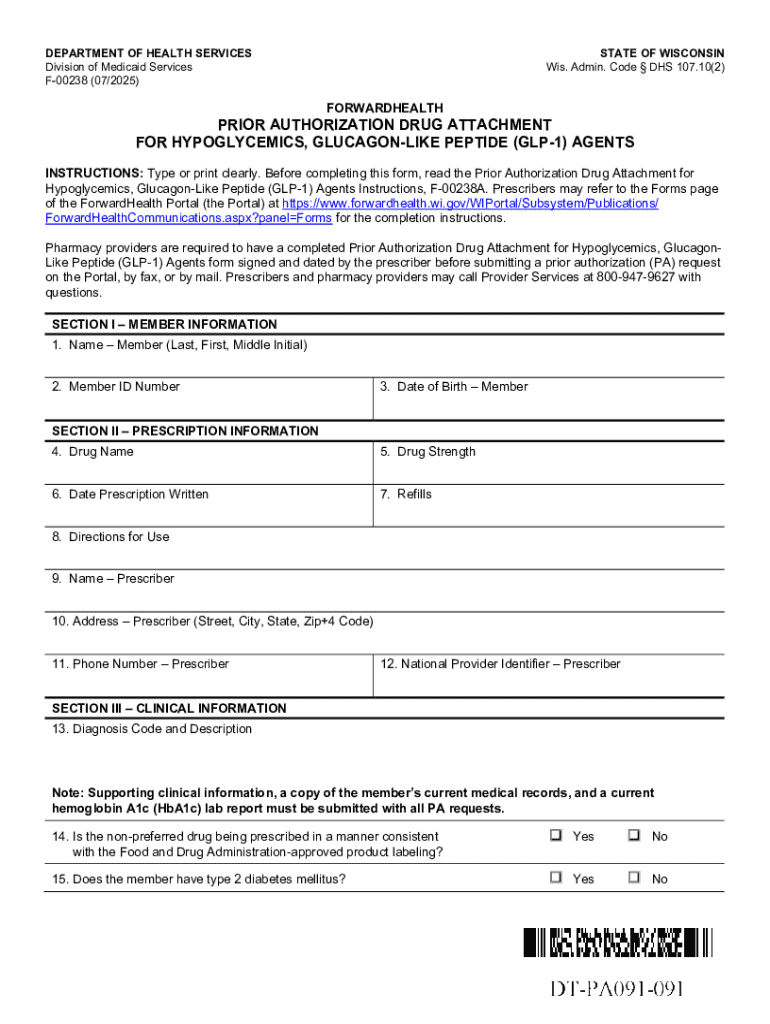
Get the free Prior Authorization Drug Attachment for Hypoglycemics, Glp-1 Agents
Get, Create, Make and Sign prior authorization drug attachment
Editing prior authorization drug attachment online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization drug attachment
How to fill out prior authorization drug attachment
Who needs prior authorization drug attachment?
Comprehensive Guide to the Prior Authorization Drug Attachment Form
Overview of prior authorization drug attachments
Prior authorization is a crucial healthcare process that requires healthcare providers to obtain approval from insurance companies before prescribing certain medications or treatments. This essential step helps to control costs and ensure appropriate care for patients. The drug attachment form plays a vital role in this process, as it provides detailed information on the requested medication, patient demographics, and clinical justification.
The primary purpose of the drug attachment form is to facilitate the communication between healthcare providers and insurers. By detailing the medical necessity of the medication, it increases the chances of approval by the insurance company. Common scenarios that trigger the need for prior authorization include high-cost medications, treatments requiring specialized care, or drugs that have specific criteria set by the insurer.
Understanding the prior authorization process
The prior authorization process can seem daunting, but breaking it down into manageable steps helps to demystify it. The workflow generally includes three main steps:
Key stakeholders in this process include the patient, who needs the medication; the provider, who submits the request; and the insurer, who makes the approval decision. Effective communication between these parties is essential for a smooth prior authorization experience.
Detailed guide to the drug attachment form
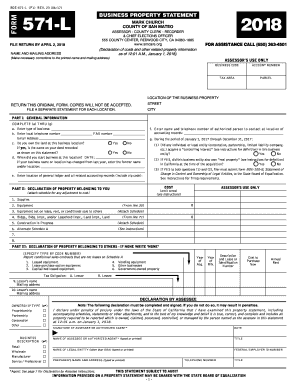
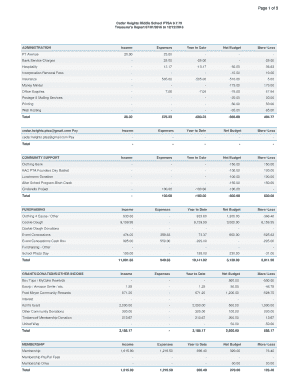
The drug attachment form consists of various sections, each designed to gather critical information about the patient, medication, and treatment history. Understanding these sections is key to successful completion. The main segments include:
When filling out each section, it's crucial to be thorough and precise. Ensure accuracy, as missing or incorrect information can lead to approval delays or denials. Always double-check the form before submission.
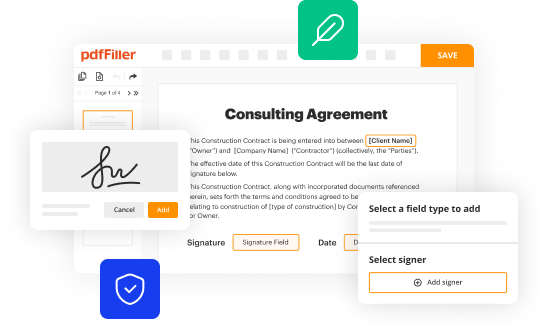
Interactive tools for form creation and management
Utilizing digital tools can significantly streamline the process of completing and submitting the prior authorization drug attachment form. One such platform is pdfFiller, which offers powerful features for editing and managing documents. Key features include:
Moreover, pdfFiller facilitates collaboration by allowing users to share forms with healthcare teams, which can improve communication and ensure that everyone is on the same page. Real-time editing features allow for quick updates, reducing the turnaround time for form completion.
Frequently asked questions (FAQs)
Understanding commonly asked questions about the prior authorization process can alleviate concerns for patients and healthcare providers alike. Here are some FAQs that often arise:
Clarification on documentation requirements is also common, as each insurer may have different criteria.
Best practices for successful submission
To increase the probability of a successful prior authorization approval, consider the following best practices:
By adhering to these practices, healthcare providers can reduce frustration and improve the approval rate.
Troubleshooting common issues
Encountering issues during the prior authorization process can be frustrating. Some common problems include:
Being proactive and prepared can make a significant difference in navigating these challenges.
Additional considerations for specific drug requests
Some medications have stricter prior authorization requirements due to their cost, potential for misuse, or specific clinical guidelines. Consider the following when dealing with such medications:
Being prepared with all necessary documentation tailored to the specific requirements can be vital for timely approval.
Future trends in prior authorizations and drug attachments
The landscape of prior authorizations and drug attachments is evolving. As regulations change, several trends are emerging:
Adapting to these trends will be critical for healthcare providers as they navigate the future landscape of medication management.
Leveraging pdfFiller for a seamless experience
pdfFiller offers a cloud-based platform ideal for managing documents like the prior authorization drug attachment form. Benefits include:
Leveraging these capabilities not only streamlines the prior authorization process but also enhances overall document management efficiency.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find prior authorization drug attachment?
Can I create an electronic signature for the prior authorization drug attachment in Chrome?
Can I edit prior authorization drug attachment on an Android device?
What is prior authorization drug attachment?
Who is required to file prior authorization drug attachment?
How to fill out prior authorization drug attachment?
What is the purpose of prior authorization drug attachment?
What information must be reported on prior authorization drug attachment?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.