Get the free Nc Medicaid Pharmacy Prior Approval Request
Get, Create, Make and Sign nc medicaid pharmacy prior



How to edit nc medicaid pharmacy prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nc medicaid pharmacy prior

How to fill out nc medicaid pharmacy prior
Who needs nc medicaid pharmacy prior?
NC Medicaid Pharmacy Prior Form: A Comprehensive Guide
Understanding NC Medicaid Pharmacy Prior Authorization
Prior authorization is a crucial component of the NC Medicaid program, designed to manage the costs and accessibility of medications. It requires providers to obtain approval from NC Medicaid before certain medications are prescribed or dispensed, ensuring that patients receive the most appropriate and cost-effective treatments.
The role of NC Medicaid in pharmacy services cannot be overstated. It aims to safeguard both patient health and the integrity of the Medicaid program by reviewing medication requests to confirm their medical necessity. This process is pivotal in ensuring that resources are utilized in an efficient manner, benefiting both the providers and the patients.
Overview of the Prior Authorization Process
The prior authorization process serves several key goals, including the promotion of safe prescribing practices and the minimization of unnecessary healthcare costs. It establishes a system of checks and balances, ensuring that patients are prescribed medications that are both therapeutically appropriate and financially viable.
Benefits extend to patients and providers alike, including streamlined processes that can enhance care coordination and improve patient outcomes. By ensuring that only necessary medications are covered, prior authorization can decrease instances of over-medication and potential adverse drug reactions.
Eligibility criteria for NC Medicaid Pharmacy Prior Authorization
Eligibility for NC Medicaid pharmacy prior authorization encompasses various participants in the healthcare system. Primary eligibility includes Medicaid members who are receiving specific medications that require authorization. Medicaid recipients are often in need of effective therapies that must first be evaluated.
From the provider's perspective, healthcare professionals authorized to write prescriptions must also understand the criteria that qualify specific medications for prior authorization. This includes awareness of the forms needed to initiate requests.
Conditions that require prior authorization
Certain conditions and medications necessitate prior authorization under NC Medicaid. Specific high-cost or unique therapies, as well as new and experimental treatments, must be evaluated before patients can access these medications. Ensuring the prescribed therapy aligns with clinical guidelines and has been shown to effectively treat the condition at hand is essential.
In addition, exceptions may apply for patients undergoing specific levels of care or those with unique medical conditions. Understanding these nuances is critical for providers and patients navigating the prior authorization landscape.
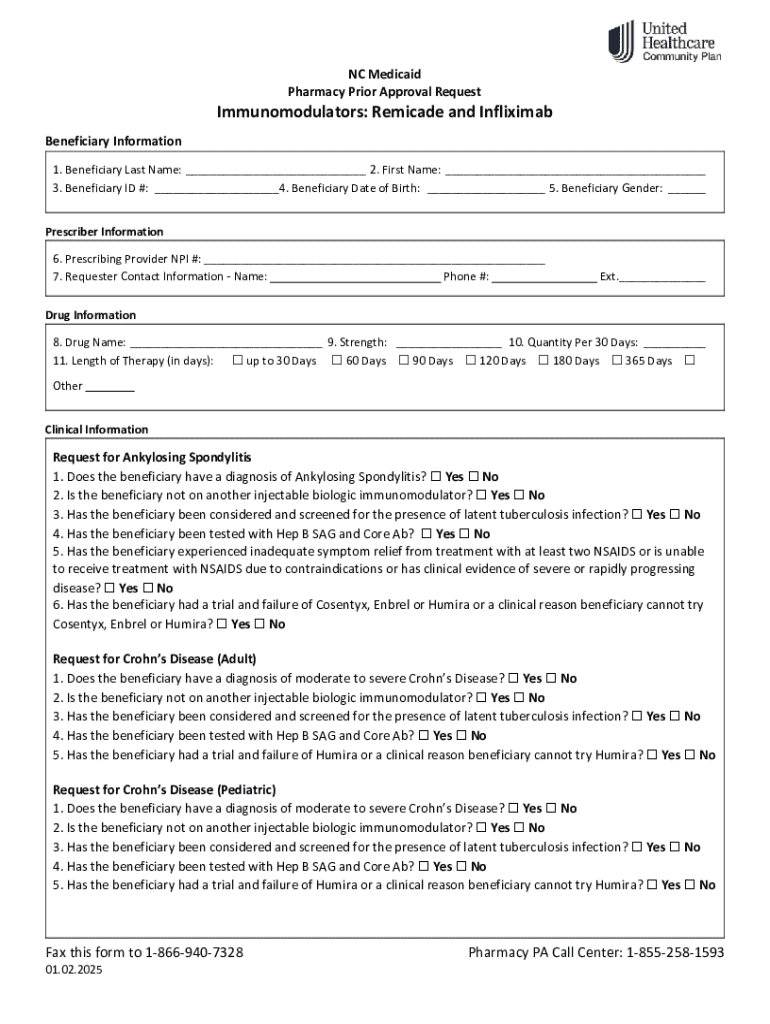
Navigating the NC Medicaid Pharmacy Prior Authorization Form
Successfully navigating the NC Medicaid pharmacy prior authorization form requires an understanding of its structure and components. Familiarity with the key sections helps healthcare providers ensure completeness and accuracy, which reduces the chances of denials or delays.
The form is typically organized into distinct sections outlining patient and provider information, as well as medication-related details. Key terminology used throughout the form should be clearly defined, allowing both providers and patients to understand requirements easily.
Step-by-step guide to completing the form
Completing the NC Medicaid pharmacy prior authorization form involves several critical steps. Beginning with patient information, the form requires accurate and complete identification of the patient, including their Medicaid identification number, contact details, and relevant medical history.
Section 2 requires detailed provider information, confirming the prescriber's credentials and contact data. In Section 3, the medications must be listed along with the clinical rationale or diagnosis justifying the request, ensuring that all information is concise and complete.
Lastly, Section 4 involves submitting supporting documentation, such as previous treatment history, lab results, or specialty assessments. Including thorough and relevant documentation enhances the likelihood of approval.
Tips for accurate form submission
To ensure a successful submission of the NC Medicaid pharmacy prior authorization form, attention to detail is paramount. Review each section carefully, as missing information or inaccurate data can lead to denials or requests for additional information, which prolongs the process.
Common errors include failing to include required supporting documentation and not clearly defining the clinical necessity for the medication. Taking the time to double-check the form before submission can save time and stress for both healthcare providers and patients.
Interacting with the prior authorization system
Submitting the NC Medicaid pharmacy prior authorization form can be accomplished through various methods, one of which is a streamlined online submission process offered through platforms like pdfFiller. This tool simplifies the form-filling experience by allowing users to edit, eSign, and manage documents easily from any device.
Alternatives to online submissions include traditional mail or fax. However, the online approach significantly reduces submission time and enhances tracking capabilities.
Tracking the status of your prior authorization
Once the form has been submitted, tracking its status is a vital step in the prior authorization process. Healthcare providers can check the status online, allowing them to stay informed and promptly respond to any requests for additional documentation or clarification.
Understanding approval and denial notifications is also crucial. Providers should familiarize themselves with common reasons for denials, such as insufficient documentation or lack of clinical evidence, enabling them to address these issues proactively.
Common challenges and solutions
Challenges are an inherent part of navigating the NC Medicaid pharmacy prior authorization process. Delays in approval can emerge due to various factors, including incomplete submissions and high volume requests. It's essential for providers to stay engaged and responsive to minimize these delays.
In instances of denied requests, understanding the appeals process is vital. Providers can often address the issues pointed out in the denial and resubmit their requests with the necessary corrections or additional documentation.
Resources for assistance
Providers looking for additional support can access various resources offered by NC Medicaid. Contacting support teams through dedicated helplines can clarify specific concerns about form submissions or prior authorization requirements. Additionally, the NC Medicaid website offers a wealth of information and help tools to guide users.
Pharmacists also play a unique role in navigating medication and prior authorization, providing essential support to both patients and providers. They can assist with medication therapy management and clarify any uncertainties in prescription coverage.
Additional information and resources
Pharmacists are integral to the prior authorization process. They frequently collaborate with both patients and providers to enhance medication adherence and optimize therapeutic outcomes. Ensuring effective communication among all parties can streamline the overall process.
Patient education is another essential factor in medication management. Understanding coverage options, alternatives, and community resources can empower patients to take an active role in their healthcare decisions. This education can include discussions about prescribed therapies and their potential implications.
Upcoming training and events
Engagement through training and events is opened to healthcare providers interested in improving their understanding of the NC Medicaid pharmacy prior authorization process. Sessions such as webinars and workshops offer avenues to explore best practices and updates in the system.
Participation in community outreach programs can also help institutions build a rapport with local populations, ensuring better access to information about Medicaid services and offerings.
Quick reference: Important links and tools
To facilitate the process of navigating the NC Medicaid pharmacy prior authorization form, here are some key resources that can streamline the user's experience. Starting with access to the NC Medicaid website, users can find the foundational guidelines and materials needed for prior authorization.
Additional tools include quick links to forms, documentation, and a provider login for easy access to personalized content and tracking. Utilizing these resources can effectively enhance the submission and follow-up process.
Feedback mechanisms
Collecting feedback is instrumental in enhancing the user experience for those engaging with the NC Medicaid pharmacy prior authorization system. Providers and patients alike can share their experiences to highlight successes and challenges, potentially informing improvements in processes.
Mechanisms for feedback may vary, but they often include surveys and direct communication with support teams. Organizations are encouraged to foster an open dialogue with users, ensuring that their input is valued and acted upon.
Language assistance and support services
Recognizing the diverse linguistic backgrounds within the NC Medicaid population, language assistance is vital. Services are available for non-English speakers, ensuring that every patient receives the information they need regarding their prior authorization.
Interpreter services and auxiliary aids can bridge communication gaps, fostering clearer understanding and collaboration among patients and providers. This support not only facilitates successful submission of prior authorization forms but also enhances the overall healthcare experience.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the nc medicaid pharmacy prior electronically in Chrome?
How do I edit nc medicaid pharmacy prior on an Android device?
How do I fill out nc medicaid pharmacy prior on an Android device?
What is nc medicaid pharmacy prior?
Who is required to file nc medicaid pharmacy prior?
How to fill out nc medicaid pharmacy prior?
What is the purpose of nc medicaid pharmacy prior?
What information must be reported on nc medicaid pharmacy prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.