Get the free Prior Authorization Request
Get, Create, Make and Sign prior authorization request



How to edit prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request

How to fill out prior authorization request
Who needs prior authorization request?
Prior Authorization Request Form - How-to Guide
Understanding prior authorization: essential insights
Prior authorization is a cost-control process utilized by health insurance providers to ensure that certain medical services, procedures, or medications are deemed medically necessary before coverage is authorized. This step is essential not only for controlling healthcare costs but also for ensuring that patients receive appropriate treatments based on their specific circumstances.
Largely used in the U.S. healthcare system, prior authorization aims to curb unnecessary spending while ensuring efficient patient care. Various stakeholders, including insurers, healthcare providers, and patients, play critical roles in this process.
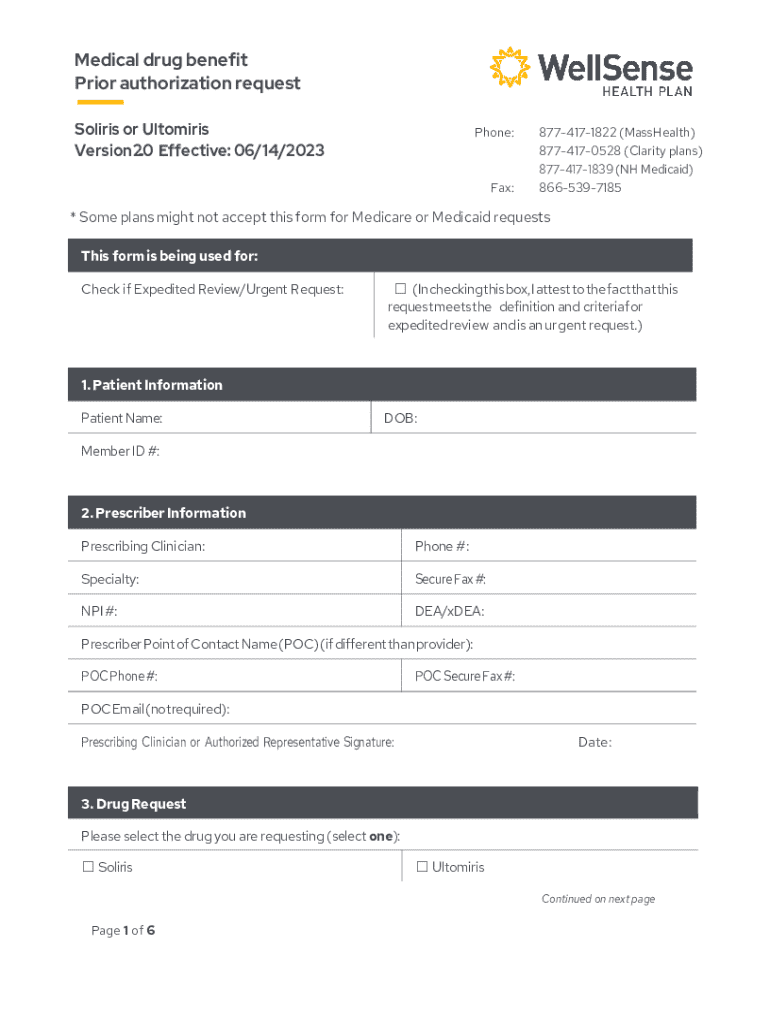
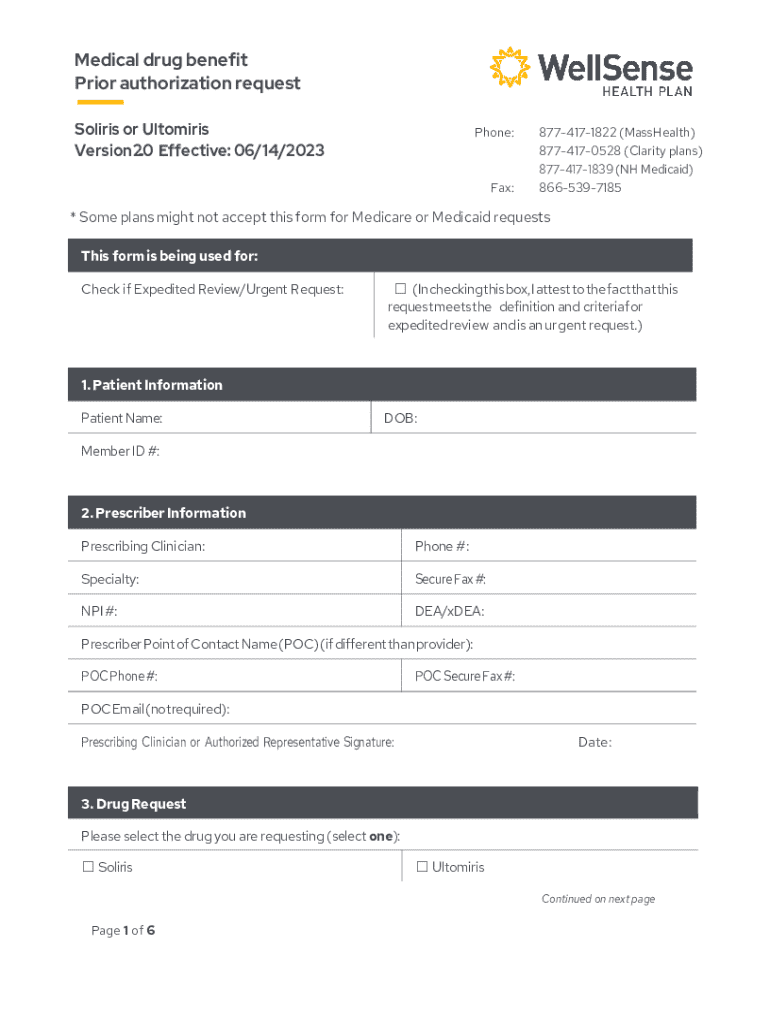
Overview of the prior authorization request form
The prior authorization request form is an official document that healthcare providers must complete and submit to insurance companies to obtain approval for a specified service or procedure. This form includes critical information about the patient, the requested treatment, and clinical justification to support the necessity of the service.
Understanding the key elements of this form is vital for ensuring a smooth approval process. Components typically include patient information (such as name and date of birth), provider information (including NPI number and contact details), and detailed descriptions of the services or medications being requested.
Step-by-step guide: completing the prior authorization request form
Filling out the prior authorization request form correctly is paramount for obtaining timely approval. To navigate this process, follow these structured steps:
Using pdfFiller to enhance your submission process
pdfFiller offers a versatile platform that enhances the prior authorization submission process, streamlining document management and collaboration. The intuitive tool allows users to edit forms seamlessly, ensuring clarity and professionalism in every submission.
The advantages of utilizing pdfFiller are numerous, providing users with enhanced functionalities like e-signing, which expedites the approval process by allowing quick consent from all required parties without the hassle of printing, signing, and rescanning documents.
How to submit your prior authorization request form
Once the prior authorization request form is accurately completed and reviewed, the next crucial step is the submission process. Understanding your submission options leads to a timely and effective authorization.
Common submission methods include electronic submissions through insurance portals, faxing the completed form, and mailing it directly to the insurance company. Each method has its pros and cons, but electronic submissions are generally faster and help maintain accurate records.
After submission: what to expect
Once the prior authorization request form has been submitted, the review process begins. The time taken for approval or denial can vary significantly based on the insurer's internal processes and the complexity of the request.
On average, insurers may take anywhere from a few days to two weeks to communicate their decision. It is essential for healthcare providers to prepare patients for varying responses and the possibility of denials.
FAQs related to prior authorization requests
As the prior authorization process can be complex and sometimes frustrating, having a clear understanding of common questions can aid in navigating it successfully.
Leveraging technology to simplify future requests
To further enhance efficiency, healthcare providers can leverage digital tools like those offered by pdfFiller when managing repetitive tasks associated with prior authorization requests.
Utilizing pdfFiller's features allows for rapid form completion for multiple requests, creating templates for commonly requested services, and ensuring that previous submission data can be easily accessed for future needs.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Where do I find prior authorization request?
Can I create an electronic signature for signing my prior authorization request in Gmail?
Can I edit prior authorization request on an iOS device?
What is prior authorization request?
Who is required to file prior authorization request?
How to fill out prior authorization request?
What is the purpose of prior authorization request?
What information must be reported on prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.