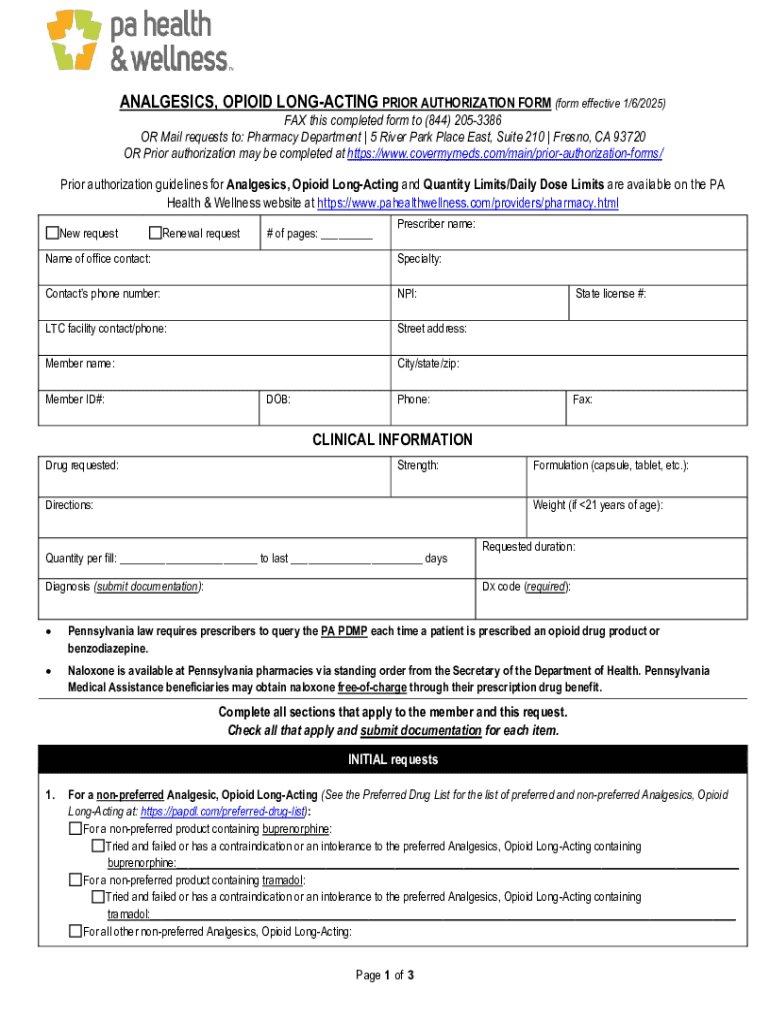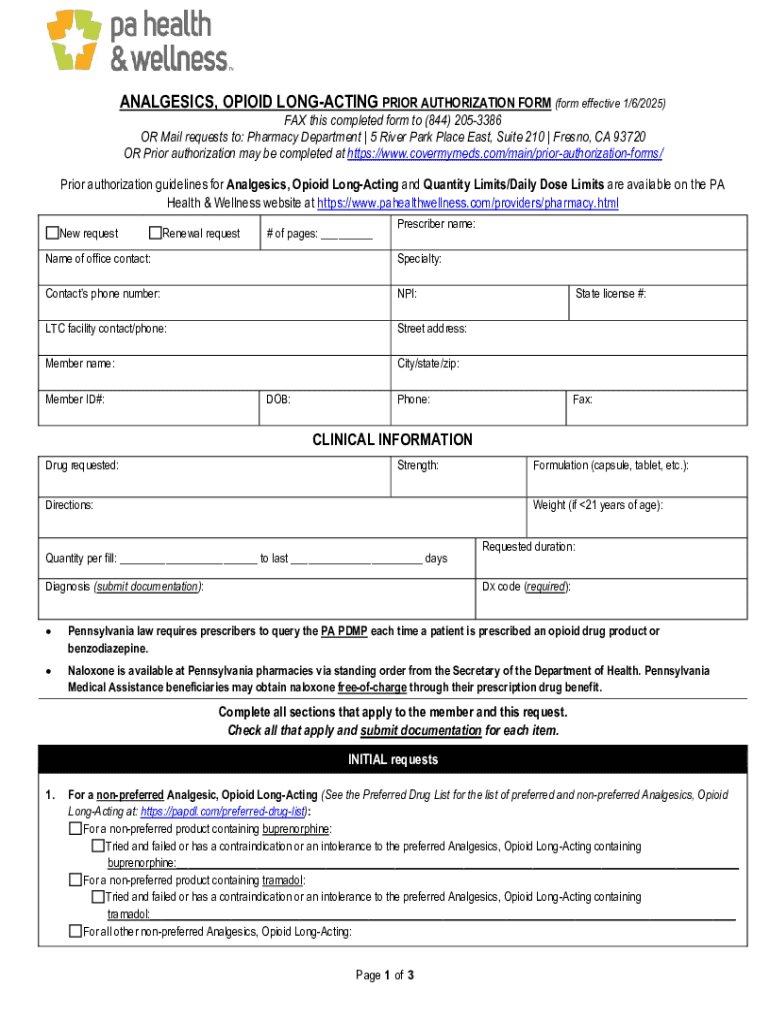
Get the free Analgesics, Opioid Long-acting Prior Authorization Form
Get, Create, Make and Sign analgesics opioid long-acting prior
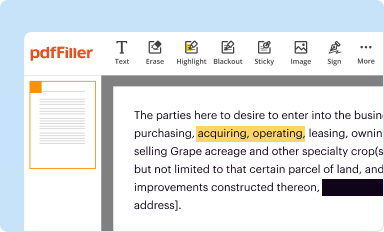
Editing analgesics opioid long-acting prior online
Uncompromising security for your PDF editing and eSignature needs
How to fill out analgesics opioid long-acting prior
How to fill out analgesics opioid long-acting prior
Who needs analgesics opioid long-acting prior?
Understanding Analgesics Opioid Long-acting Prior Form
Understanding long-acting opioids
Long-acting opioids are a crucial component in the management of chronic pain, providing sustained relief over extended periods. Unlike short-acting opioids, which offer rapid onset but require more frequent dosing, long-acting opioids are designed to release medication slowly into the bloodstream, allowing patients to experience a more consistent level of pain relief. This sustained action is particularly beneficial for individuals dealing with conditions that present ongoing pain challenges, such as cancer, fibromyalgia, or severe arthritis.
The clear distinction between long-acting and short-acting opioids lies primarily in the duration of effects. Long-acting formulations usually require intake every 12 to 24 hours, while short-acting ones may need to be taken every 4 to 6 hours. It’s essential to weigh the benefits against the limitations. Long-acting opioids can manage pain more effectively in chronic situations; however, they come with heightened risks, including potential dependence and side effects.
Importance of prior authorization
Prior authorization is a critical process in healthcare that requires physicians to obtain approval from insurers before prescribing certain medications, including long-acting opioids. This step aims to ensure that the use of these potent medications is medically justified and aligns with best practice guidelines.
The necessity for prior authorization not only helps mitigate misuse and abuse associated with opioid prescriptions but also ensures the appropriate allocation of healthcare resources. It serves as a pivotal checkpoint to balance effective pain management with the overarching goal of patient safety and cost management. Insurers utilize it to verify that patients have explored alternative treatments that might be more suitable before resorting to long-acting opioids.
Key components of the long-acting opioid prior authorization form
When it comes to filling out the long-acting opioid prior authorization form, certain crucial details must be included to ensure a smooth approval process. This form typically requests comprehensive patient information, including personal details such as name, age, and medical history pertinent to pain management. Additionally, it requires data from the prescribing physician, ensuring that the medical necessity for the opioid therapy is properly documented.
Medication-specific information is also essential, outlining the exact long-acting opioids being prescribed, their dosages, and the justification for their selection based on the patient’s unique pain management needs. This section may also necessitate the submission of additional supporting documents, such as medical records or treatment history, especially for patients who have undergone varied therapies prior to opioid initiation.
Step-by-step guide to filling out the prior authorization form
Filling out the prior authorization form accurately is critical for a successful outcome. Start by gathering all necessary information, ensuring that you have access to patient records, medication history, and any recent lab or imaging studies that may support the medical necessity of the prescription. Once you have compiled the necessary documents, proceed to the following steps.
Step 1 involves completing the patient information section with meticulous attention to detail, providing accurate personal information and any relevant medical history to substantiate the pain management claims. In Step 2, include comprehensive data about the physician's credentials, including contact details, to allow for follow-up verification. Step 3 covers the specific medication you intend to prescribe; ensure you provide the correct dosage and length of therapy.
Step 4 emphasizes the importance of crafting a solid justification for the chosen long-acting opioid, outlining why it is necessary over other alternatives. Finally, Step 5 requires a thorough review of the entire form for any possible errors before submission, either electronically or via fax.
Common mistakes to avoid
Navigating the prior authorization process can be tricky, and avoiding common pitfalls is essential for maximizing your chances of approval. One significant mistake is providing incomplete information, which can lead to delays or outright denials. Always ensure that every required field is filled correctly; even minor inaccuracies can have substantial consequences.
Improper or vague justifications for requesting a long-acting opioid can also hinder approval chances. It is crucial to specifically articulate the clinical necessity for the medication based on the patient’s condition and previous treatments. Additionally, delayed submissions due to indecision or lack of timely documentation can negatively impact patient care, rendering the entire process ineffective.
Tracking the approval process
Once the prior authorization form has been submitted, it’s essential to understand what to expect regarding the approval process. The typical timeline for review and response can vary significantly based on the insurance provider but often ranges from a few hours to several days. Insurers may require further clarification or additional documentation during their review, which can extend these timelines.
If the request is denied, there are clear steps to follow. Most insurance companies provide a means to appeal denials if the prescribing physician can supply additional evidence or more compelling justifications. Maintaining clear lines of communication with the insurance provider can facilitate a more seamless process and aid in addressing any questions that arise.
Resources for support
Navigating the complexities of a long-acting opioid prior authorization form can be daunting. If assistance is needed, professionals can reach out to specific hotline numbers for help during the form completion process. Most health insurance companies and hospitals offer resources dedicated to assisting in managing prior authorization inquiries effectively.
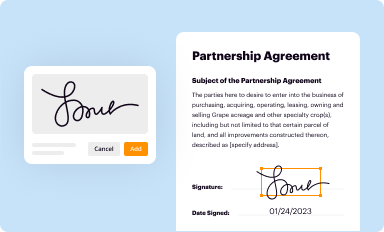
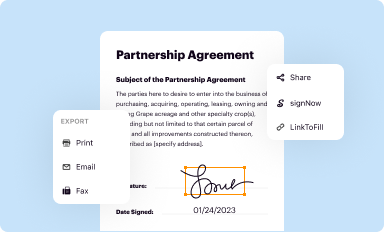
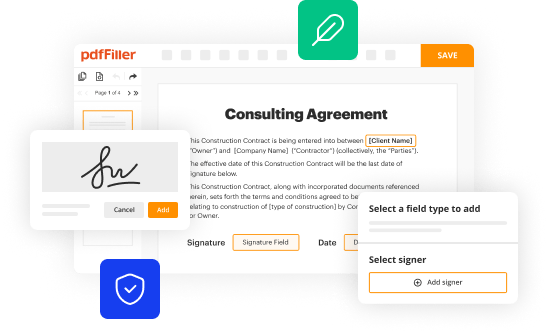
Additionally, utilizing digital tools like pdfFiller can make the form-filling experience smoother. This platform provides interactive features that aid users in uploading, editing, and managing the prior authorization documents efficiently and ensures a streamlined collaboration among healthcare teams.
Benefits of using pdfFiller for your documentation needs
pdfFiller emerges as a versatile solution for handling prior authorization forms, streamlining the entire document management process. Its cloud-based platform allows users to access and manage their documents from virtually anywhere, making it easy to fill out, edit, and submit forms without being tied to a specific location. This flexibility is particularly useful in healthcare settings where time and mobility are critical.
The platform further enhances productivity with eSignature capabilities, enabling quick and easy acquisition of necessary signatures electronically. This feature not only saves time but also contributes to a more efficient workflow in busy medical environments. Additionally, pdfFiller fosters collaboration among healthcare teams through shared document editing features, allowing multiple users to work on the same form simultaneously, enhancing communication and reducing errors.
FAQs about long-acting opioid prior authorization
Frequently asked questions regarding the prior authorization process often revolve around eligibility requirements and specific procedural nuances. Patients or healthcare providers may wonder what constitutes eligibility for long-acting opioid prescriptions or what documentation is necessary to support such requests. Addressing these inquiries upfront can significantly demystify the authorization process and provide clarity.
For example, a common situation might involve a patient switching from short-acting opioids to a long-acting regimen due to escalating pain needs. Understanding the justification required in these cases can prepare healthcare providers for successful approvals. Resources such as dedicated FAQs on insurer websites or even at pdfFiller can empower users with the knowledge needed to navigate the system effectively.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify analgesics opioid long-acting prior without leaving Google Drive?
How do I make changes in analgesics opioid long-acting prior?
Can I create an electronic signature for signing my analgesics opioid long-acting prior in Gmail?
What is analgesics opioid long-acting prior?
Who is required to file analgesics opioid long-acting prior?
How to fill out analgesics opioid long-acting prior?
What is the purpose of analgesics opioid long-acting prior?
What information must be reported on analgesics opioid long-acting prior?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.