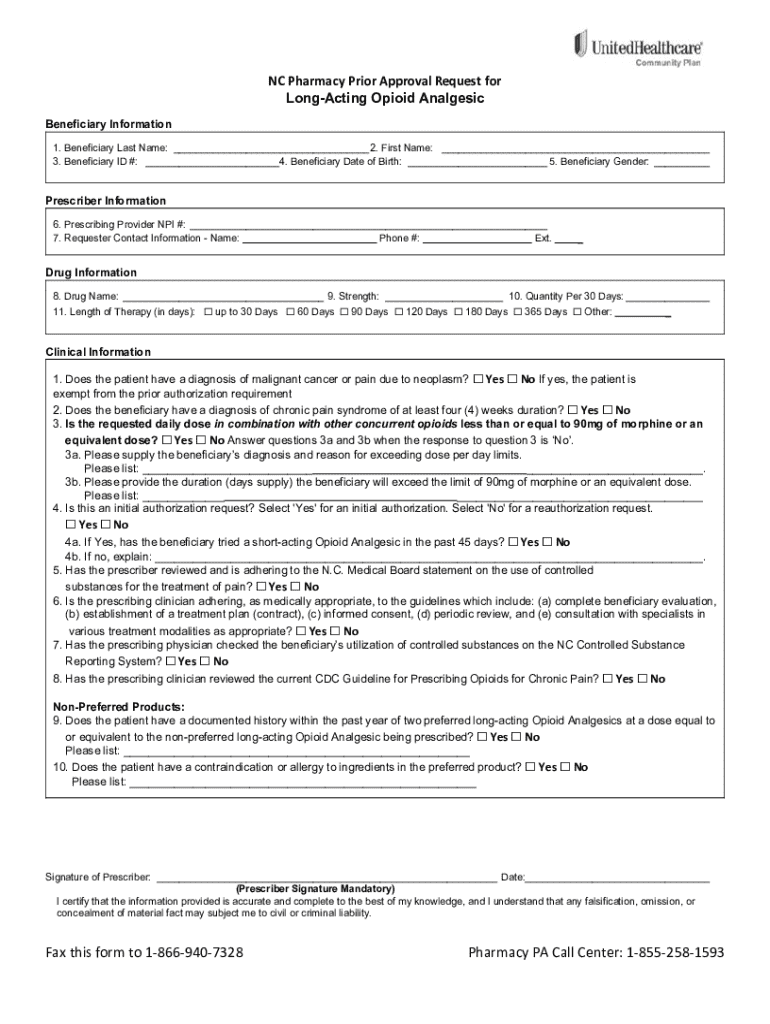
Get the free Nc Pharmacy Prior Approval Request for Long-acting Opioid Analgesic
Get, Create, Make and Sign nc pharmacy prior approval



How to edit nc pharmacy prior approval online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nc pharmacy prior approval

How to fill out nc pharmacy prior approval
Who needs nc pharmacy prior approval?
A Comprehensive Guide to the NC Pharmacy Prior Approval Form
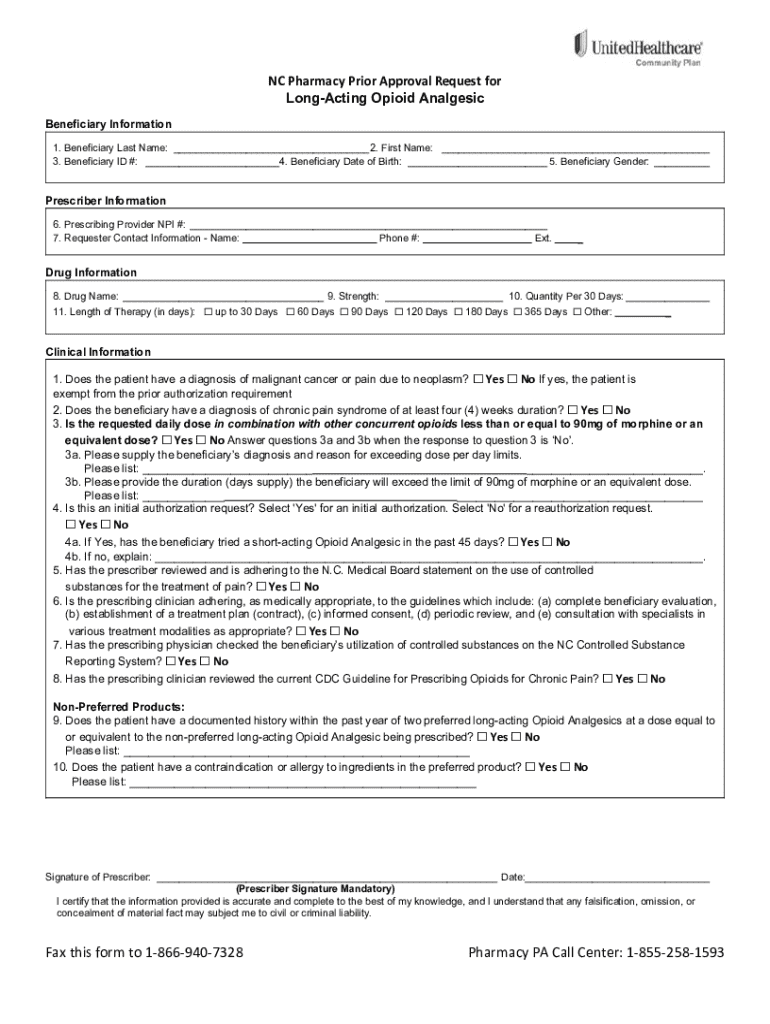
Understanding the NC Pharmacy Prior Approval Form
The NC Pharmacy Prior Approval Form is a vital document that healthcare providers in North Carolina must submit to gain approval for certain medications before they can be dispensed to patients. This form is particularly necessary for drugs that require special authorization, often due to their high cost or specific clinical indications. The importance of this process cannot be understated, as it ensures that patients receive appropriate medications covered by their insurance, while also promoting responsible use of healthcare resources.
Key terminology related to this form includes 'prior approval,' which refers to the required permission from an insurance company before it will cover a medication; 'medical necessity,' which signifies that a drug is essential for treating a patient's condition; and 'formulary,' which is the list of covered drugs by a particular insurance plan. Understanding these terms helps navigate the approval process more effectively.
Who Needs the NC Pharmacy Prior Approval Form?
Several stakeholders are involved in the NC Pharmacy Prior Approval process. Primary among them are patients, who depend on prescribed medications for their health. They must ensure that their medications are approved for coverage to avoid high out-of-pocket expenses.
Healthcare providers, including physicians and pharmacists, play a pivotal role in filling out and submitting the form. Physicians must articulate the medical need for the prescribed medication, while pharmacists help procure and verify that approval has been granted for dispensing the drug. Lastly, insurance companies and payers are crucial as they evaluate the requests and make decisions based on established guidelines.
Steps to prepare for filling out the NC Pharmacy Prior Approval Form
Before filling out the NC Pharmacy Prior Approval Form, it is essential to gather all necessary information efficiently. Start with the patient’s information, which includes their full name, date of birth, insurance details, and any pertinent identification numbers. Accurate data here will avoid delays.
Next, ensure that you have detailed medication information at hand. This should include the drug name, dosage, and the quantity requested. Beyond simply listing these details, understanding the clinical rationale for the medication will be vital. Additionally, provider information, including the name, contact details, and specialty of the prescribing doctor, is crucial for accurate authorization.
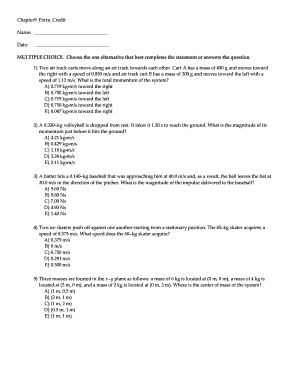
Detailed guide to filling out the NC Pharmacy Prior Approval Form
Filling out the NC Pharmacy Prior Approval Form requires attention to detail. The form is divided into several sections that must be carefully completed. The first is the Patient Information Section, where you provide basic patient details, ensuring all information is accurate.
In the Medication Requested Section, specify the medication name, its dosage, and the quantity. The Clinical Information Section must include relevant diagnosis and any prior therapies tried, ensuring to highlight the 'medical necessity' of the drug. Finally, the Provider Information Section should have the prescribing physician’s contact details for follow-up communication.
While filling out the form, common mistakes include providing incomplete information, missing signatures, or failing to specify the therapy rationale. Always double-check the completed form for accuracy.
Submitting the NC Pharmacy Prior Approval Form
Once the form is completed, the next step is submission. Accepted submission methods include online submission through your insurance company’s portal, mailing a hard copy to the appropriate address, or faxing the completed form directly. Each method has its own benefits, and familiarizing yourself with these can streamline the process.
It’s crucial to be aware of submission deadlines as well. Adhering to these timelines can significantly influence the approval process and ultimately affect patient care. For many insurance companies, approvals can take anywhere from a few days to a couple of weeks, so timely submission is vital.
Frequently asked questions (FAQs)
Approval for the NC Pharmacy Prior Approval Form can sometimes be denied, leaving patients and providers in a challenging situation. If your prior approval is denied, the first step is to carefully review the denial letter, which should explain the rationale behind the decision. Understanding the reasons allows for a more effective appeal.
To appeal a denied request, gather supporting documentation that may reinforce the necessity of the medication. This documentation can include clinical notes from the prescribing physician or additional evidence supporting the treatment plan. Approval notifications typically arrive within a specified timeframe, so understanding this can help manage patient expectations.
Tools and resources for managing your NC Pharmacy Prior Approval Form
Managing the NC Pharmacy Prior Approval Form efficiently can greatly alleviate the associated stress. Tools such as interactive forms available on pdfFiller provide a streamlined approach to completing necessary documentation. These forms allow for easy editing and digital signatures, reducing the need for physical copies.
Collaboration with your healthcare team is also essential. Establishing an open line of communication can ensure that all relevant parties are informed of the approval status and any required follow-ups. Following up with insurance companies about submitted forms can avoid unnecessary delays, especially as timelines for approvals continue to evolve.
Real-world scenarios: Success stories and challenges
Many patients have successfully navigated the NC Pharmacy Prior Approval process, resulting in receiving necessary medications promptly. For example, a patient diagnosed with a chronic condition successfully received approval by closely working with their healthcare provider to ensure all required documentation was submitted correctly. Such success stories highlight the importance of thoroughness and communication in the process.
However, challenges persist. Providers often face hurdles such as changing insurance policies or confusion around what documentation is required. Overcoming these challenges requires persistence and a strong partnership with a dedicated healthcare team as well as utilizing innovative tools provided by services like pdfFiller.
pdfFiller: Your go-to resource for document management
pdfFiller stands out as a solutions-oriented platform for managing your NC Pharmacy Prior Approval Form and other healthcare documents. Its features cater specifically to the intricacies involved in obtaining prior authorizations. Users can easily fill, edit, and share their documents, ensuring that the process remains swift and efficient.
Using a cloud-based platform such as pdfFiller enables healthcare teams to streamline their document workflow. This not only saves time but also reduces administrative burdens, allowing providers to focus more on patient care rather than paperwork.
Contacting support for assistance with the NC Pharmacy Prior Approval Form
When navigating the complexities of the NC Pharmacy Prior Approval Form, you may encounter questions or issues. In such cases, reaching out for support can be invaluable. pdfFiller offers various support channels, including a comprehensive help center that provides answers to common inquiries surrounding form completion and submission.
Additionally, live chat functions enable real-time communication with customer service representatives who can assist with urgent needs. There’s also a dedicated customer service phone line for more detailed inquiries. Knowing when to seek help can make a critical difference, especially when facing common issues like submission errors or additional documentation requests.
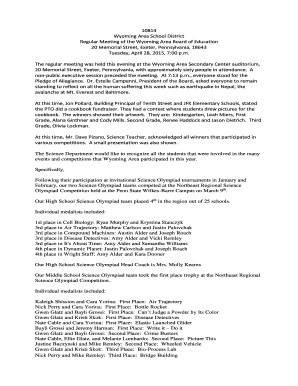
Stay informed: Updates related to NC Pharmacy and prior approval processes
Staying informed about updates related to the NC Pharmacy Prior Approval processes ensures that patients and providers remain compliant with the latest requirements. Regulatory changes can affect what medications require prior approval or the timeline associated with the approval process, making it essential to keep abreast of these developments.
Participating in educational events and training opportunities related to the NC Pharmacy processes can also enhance understanding and efficiency in completing the prior approval form. Engaging with professional organizations or subscribing to updates from healthcare regulators can further support ongoing education in this area.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit nc pharmacy prior approval from Google Drive?
Can I sign the nc pharmacy prior approval electronically in Chrome?
Can I edit nc pharmacy prior approval on an Android device?
What is nc pharmacy prior approval?
Who is required to file nc pharmacy prior approval?
How to fill out nc pharmacy prior approval?
What is the purpose of nc pharmacy prior approval?
What information must be reported on nc pharmacy prior approval?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.