Get the free Consent for Provider to File an Appeal on a Member’s Behalf
Get, Create, Make and Sign consent for provider to
Editing consent for provider to online
Uncompromising security for your PDF editing and eSignature needs
How to fill out consent for provider to
How to fill out consent for provider to
Who needs consent for provider to?
Consent for Provider to Form: A Comprehensive Guide
Overview of provider consent forms
Provider consent forms are official documents that obtain permission from patients or clients, allowing healthcare providers or service organizations to proceed with specific treatments or services. These forms play a crucial role in various sectors, primarily in healthcare and legal fields, ensuring that individuals understand the scope of procedures they consent to. The importance of consent cannot be overstated; it acts as a safeguard against potential legal implications, ensuring that providers adhere to ethical standards and respect patient rights.
Key elements found in a consent form typically include the patient’s personal information, a detailed description of procedures or treatments being offered, potential risks, benefits, alternative options, legal requirements, and the need for patient signatures. This structured approach ensures that consent is informed, allowing individuals to make educated decisions about their care.
Understanding the purpose of consent forms
Consent is necessary in numerous contexts to uphold an individual’s autonomy. In healthcare, it provides patients with the right to understand and agree to their treatment plans, whereas in legal situations, it validates agreements and permits actions to be taken. Furthermore, obtaining consent helps protect providers by minimizing the risk of litigation due to misunderstandings or unauthorized treatments.
The legal implications of obtaining consent are significant; failure to secure proper consent can lead to malpractice claims or disciplinary actions against providers. Ethically, the consent process encourages practitioners to engage with patients openly, fostering a trusting relationship. This relationship is vital in promoting patient satisfaction and outcomes, as patients who feel included in their care decisions are often more engaged in their recovery.
Initiating the consent process
Identifying when consent is needed is the first critical step in the consent process. This depends on the type of procedure or service being provided, as well as the legal requirements within a given jurisdiction. Providers are responsible for effectively communicating the importance of the consent form to their patients, ensuring that they understand what they are agreeing to.
A crucial aspect of the consent process is assessing a patient's or client's understanding. Providers should engage in a dialogue, inviting questions and ensuring that the individual comprehends the risks and benefits outlined. This confirmation strengthens the legitimacy of the consent obtained, reducing the likelihood of disputes or misunderstandings in the future.
Components of a comprehensive consent form
A well-structured consent form consists of various components that ensure clarity and thoroughness. Here are key elements included in a comprehensive consent form:
These components not only protect the provider but also empower the patient, ensuring they have access to all necessary information to make informed decisions regarding their care. Taking the time to create robust consent forms can significantly diminish legal risks and enhance the patient experience.
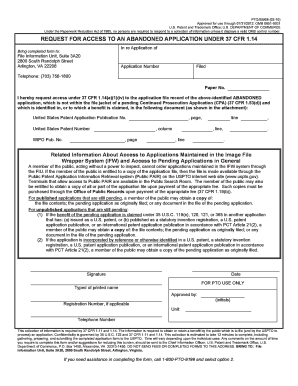
The process of filling out a consent form
Filling out a consent form should be a straightforward process, yet attention must be paid to detail to avoid common mistakes. Here’s a step-by-step guide to ensure proper completion of the form:
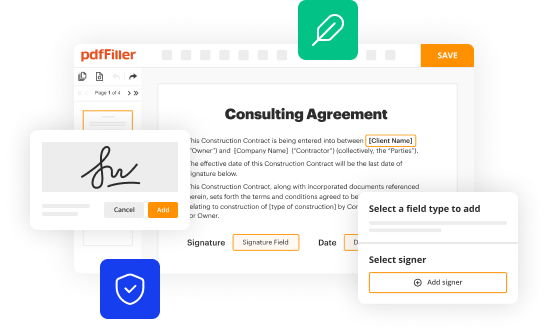
Common mistakes to avoid while filling out consent forms include using overly complex language, omitting critical information, or not allowing adequate time for the patient to read and comprehend the form. Tools like pdfFiller can streamline the editing process and facilitate easy form completion, reducing the risk of these errors.
Managing and storing consent forms
Once consent forms are completed, managing and storing them correctly is vital to maintain compliance and accessibility. Best practices for document management include organizing files systematically, using reliable digital platforms, and ensuring backup copies are available.
Compliance with privacy laws, such as HIPAA, is crucial in managing consent forms. Providers must ensure that personal health information is protected, and all consent processes adhere to these regulations to avoid potential penalties.
Special considerations in consent forms
Informed consent becomes even more nuanced in specific situations, such as when dealing with minors or individuals who are incapacitated. Here, it is essential for providers to ensure that proper guardians or legal representatives complete consent forms, reinforcing the necessity for clear communication and ethical standards in the consent process.
Recognizing and accommodating diverse cultural perspectives during the consent process can enhance patient satisfaction and trust. Providers must remain vigilant regarding the varying interpretations of consent across different cultures, adapting their approach to effectively meet the needs of all patients.
FAQs about provider consent forms
Providers often have questions regarding consent forms, particularly about legal requirements and the acceptance of electronic signatures. Questions such as these highlight the necessity for clarity in the consent process:
Addressing these questions not only reinforces a provider's understanding of best practices but also reassures patients about the integrity of the consent process.
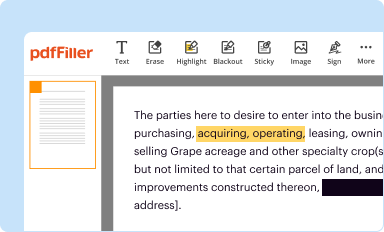
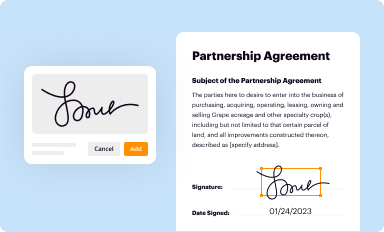
Enhancing the consent experience with technology
pdfFiller empowers teams to create and manage electronic consent forms effortlessly, addressing many of the challenges faced today. By leveraging cloud-based solutions, users can access documents from any device, making it easier to obtain and manage consent efficiently.
These advancements not only streamline the consent process but also enhance compliance and improve the overall patient experience, allowing healthcare providers to focus more on delivering quality care rather than getting bogged down in paperwork.
Summary of best practices for obtaining consent
Obtaining consent is a multifaceted process that requires careful consideration of various factors. Key takeaways from this guide include the importance of clear communication, thorough documentation, and the respectful treatment of patients’ rights. Providers should regularly review their consent practices to ensure compliance with evolving laws and ethical standards.
A commitment to these best practices will lead to better patient-provider relationships and improved healthcare outcomes, ultimately benefiting all parties involved in the consent process.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit consent for provider to from Google Drive?
How can I send consent for provider to to be eSigned by others?
Can I edit consent for provider to on an Android device?
What is consent for provider to?
Who is required to file consent for provider to?
How to fill out consent for provider to?
What is the purpose of consent for provider to?
What information must be reported on consent for provider to?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.