Get the free New Mexico Prior Authorization/statement of Medical Necessity/order Form
Get, Create, Make and Sign new mexico prior authorizationstatement
How to edit new mexico prior authorizationstatement online
Uncompromising security for your PDF editing and eSignature needs
How to fill out new mexico prior authorizationstatement
How to fill out new mexico prior authorizationstatement
Who needs new mexico prior authorizationstatement?
Understanding the New Mexico Prior Authorization Statement Form
Understanding prior authorization in New Mexico
Prior authorization is a critical process in the healthcare system that serves as a mechanism for ensuring that patients receive necessary medical services in a timely manner while managing healthcare costs effectively. In New Mexico, the prior authorization process requires healthcare providers to seek approval from insurance companies before delivering certain services or medications. This ensures that treatments align with the patient's medical needs and that they receive care that is both necessary and appropriate.
The importance of prior authorization cannot be overstated as it helps in curtailing unnecessary treatments that may lead to exorbitant costs for both patients and insurers. The process can also serve as a check against the overutilization of healthcare services, fostering better healthcare management overall.
Regulatory framework
In New Mexico, the prior authorization process is governed by a myriad of laws and regulations shaped by both state and federal mandates. The New Mexico Taxation and Revenue Department, along with the New Mexico Human Services Department, play vital roles in monitoring and regulating this process. These agencies ensure that healthcare providers comply with the standards set forth regarding those procedures requiring prior authorization.
Key regulations such as the New Mexico Insurance Code outline the necessary stipulations insurance providers must adhere to. This collaborative oversight ensures that the system functions smoothly, protecting both the patients' rights to necessary care and the insurance company's obligations to manage costs.
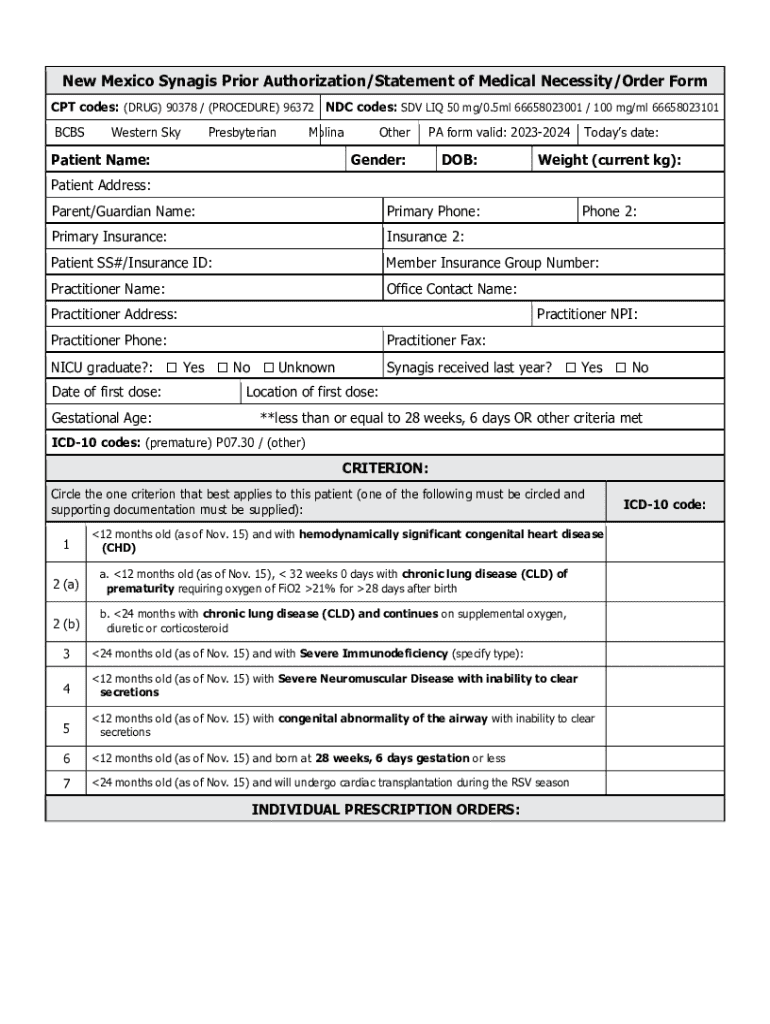
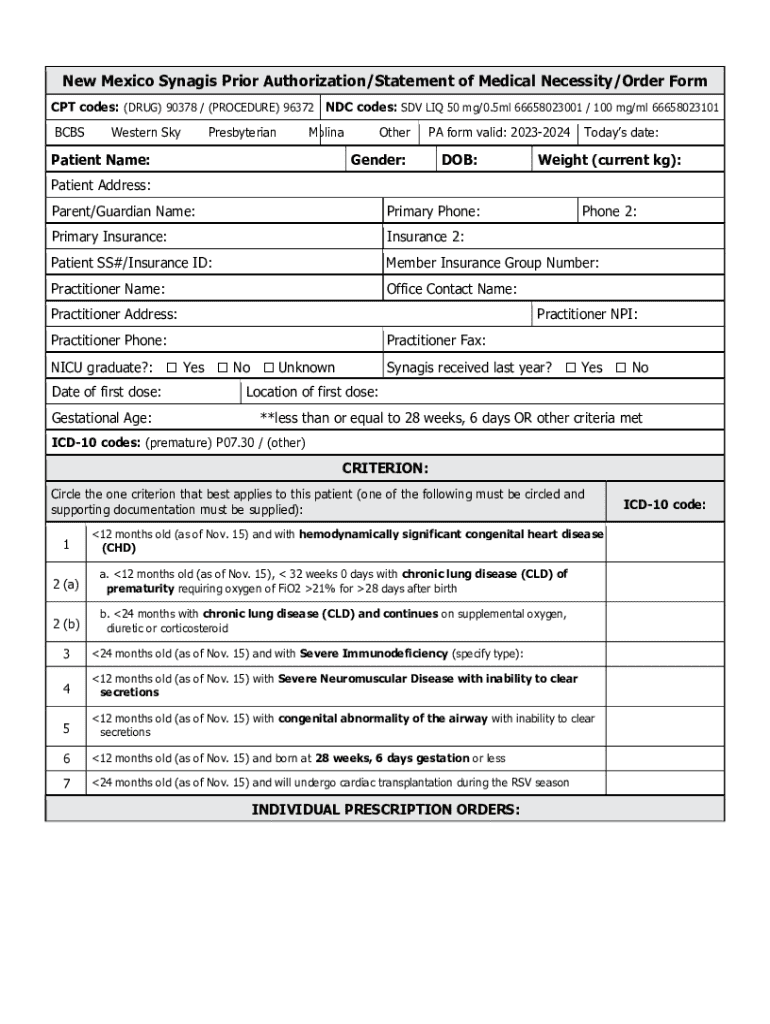
The New Mexico prior authorization statement form
The New Mexico Prior Authorization Statement Form is a standardized document used by medical providers in requesting prior approval for specific services or medications from insurance companies. This form is crucial in establishing whether a patient is eligible for the intended treatment based on their individual health circumstances and the insurance policy guidelines.
There are various scenarios wherein this form is necessary: for example, when a physician prescribes high-cost medications, or when specific diagnostic testing is required. Utilizing the form appropriately helps streamline approval processes and speeds up the overall treatment timeline.
Key components of the form
The New Mexico Prior Authorization Statement Form contains essential sections that require detailed information from both the patient and the healthcare provider. Typically, the form includes:
Common errors to avoid include providing inaccurate patient information, failing to include necessary supporting documents, and neglecting to sign the form, as these oversights can lead to delays or denials in authorization.
Step-by-step guide to completing the New Mexico prior authorization statement form
Completing the New Mexico Prior Authorization Statement Form requires careful attention to detail. Here’s a step-by-step approach:
Preparation steps
Before filling out the form, gather all necessary documentation. This includes the patient's insurance details, relevant medical history, and any previous authorization requests. Ensuring all information is current can help eliminate errors.
Additionally, confirm the specifics of the service or medication being requested and ensure that it complies with the patient's coverage policy.
Detailed instructions on filling out the form
The form will typically be divided into several sections. Here’s a breakdown of what to complete in each section:
Always review entries for accuracy and completeness before proceeding to submission.
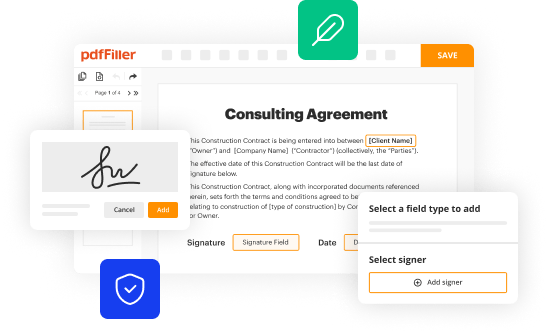
Editing the New Mexico prior authorization statement form with pdfFiller
pdfFiller provides a user-friendly platform for editing the New Mexico Prior Authorization Statement Form. To access the form on pdfFiller, navigate to the website and use the search feature to find the specific form you need. Once accessed, you can easily begin editing it digitally.
Features of pdfFiller for form editing
The platform offers several features that enhance your ability to complete the form accurately, including:
These functionalities ensure efficient workflow for both individuals and teams, making document management more straightforward.
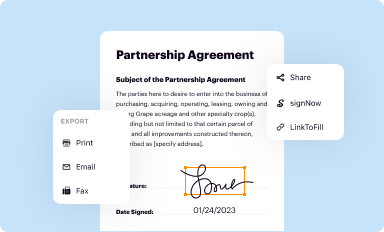
Signing and submitting the New Mexico prior authorization statement form
Once the form is completed, it must be signed before submission. Utilizing pdfFiller, you can electronically sign the form with ease. This process not only simplifies the signing procedure but also adheres to legal standards set forth in New Mexico regarding eSignatures.
Submission process
After signing, ensure you have the correct submission address for the insurance company involved. This may require validating the information on their website or through direct contact. Typically, forms can be submitted via fax or electronic submission portals, depending on the insurer's protocols.
After submission, it's advisable to follow up with the insurance provider to verify receipt and check the status of the authorization.
Managing prior authorizations
Managing the prior authorization process effectively can improve patient outcomes considerably. One way to do this is by tracking the status of your authorization. pdfFiller allows you to keep a digital record and monitor the submissions efficiently.
Handling denials and appeals
In the event that an authorization is denied, it’s important to understand the steps you should take next. Begin by reviewing the reason for denial provided by the insurance company. Often, denials can stem from missing documentation or policy exclusions.
To file an appeal in New Mexico, you’ll typically need to submit a written request outlining the grounds for the appeal along with any supporting documents. Resources are available through your insurance provider for guidance on how to proceed with the appeals process.
Common questions and troubleshooting
Users often have questions or face challenges while completing the New Mexico Prior Authorization Statement Form. Some of the most frequently encountered issues include difficulty in locating the form, confusion regarding completion requirements, and delays in processing times.
To address these common concerns:
Additional tools and resources
pdfFiller offers users access to interactive tools and templates specifically designed for managing healthcare documentation effectively. These resources simplify the process of filling out and submitting forms.
Additionally, external resources are available for both patients and providers needing assistance with navigating the prior authorization landscape. Making connections with support groups, healthcare attorney services, and patient advocacy organizations can provide additional support and insights.
Benefits of using pdfFiller for prior authorization forms
Choosing pdfFiller as your document management solution for the New Mexico Prior Authorization Statement Form comes with several benefits. One major advantage is seamless document management; the cloud-based nature of the platform allows users to create, edit, and access forms from any location. This means healthcare providers can complete necessary documentation without being tied to a specific workplace.
Furthermore, with enhanced collaboration tools, team members can work together in real-time, ensuring that all necessary information is accurately included and up to date. This collective approach not only increases efficiency but also reduces the potential for errors in form submission.
Finally, the platform prioritizes the security and compliance of sensitive information. By utilizing pdfFiller, users can feel confident that they are managing documents in a way that meets the required legal standards while safeguarding patient information.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in new mexico prior authorizationstatement without leaving Chrome?
How do I edit new mexico prior authorizationstatement on an Android device?
How do I fill out new mexico prior authorizationstatement on an Android device?
What is new mexico prior authorization statement?
Who is required to file new mexico prior authorization statement?
How to fill out new mexico prior authorization statement?
What is the purpose of new mexico prior authorization statement?
What information must be reported on new mexico prior authorization statement?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.