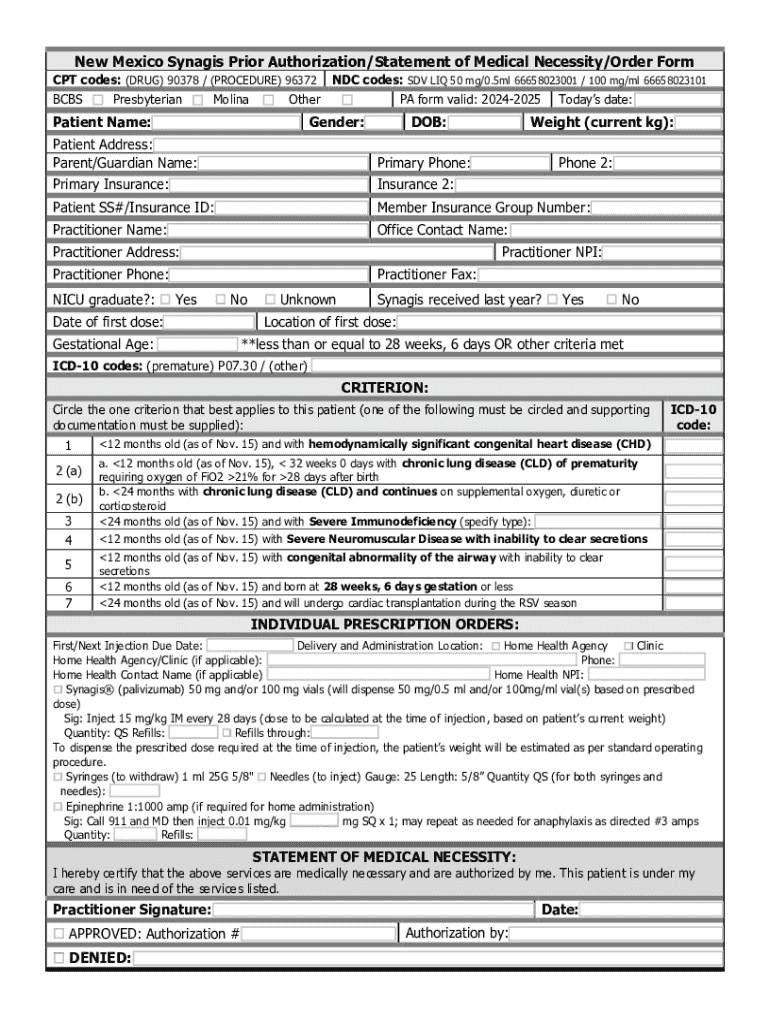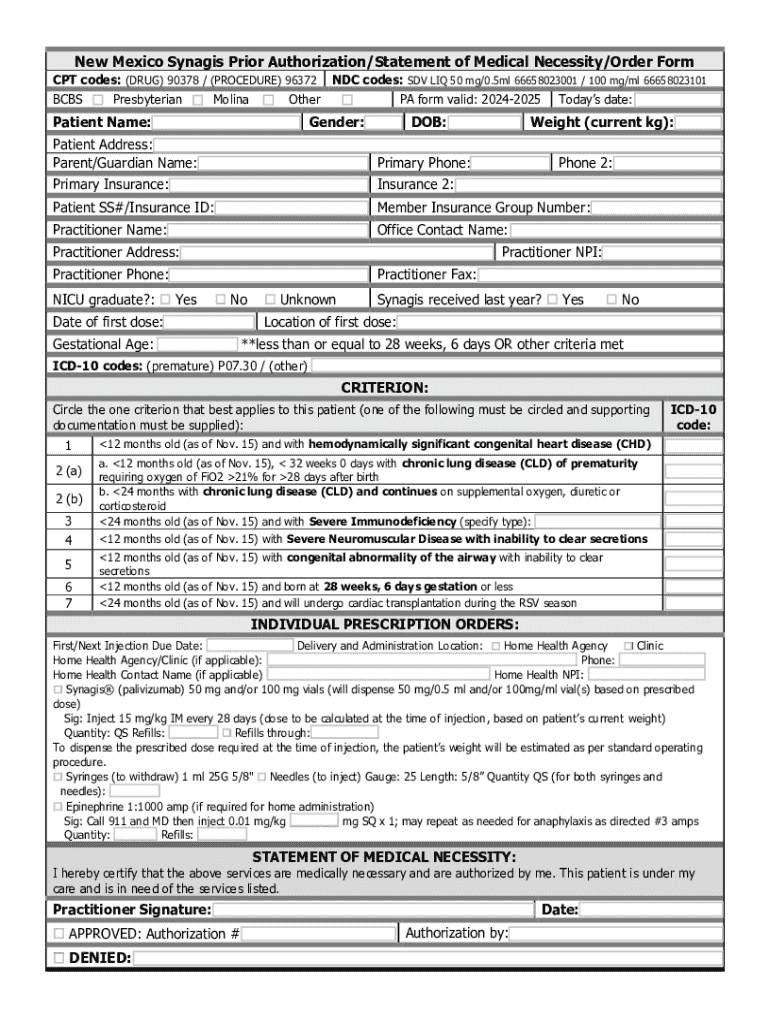
Get the free New Mexico Prior Authorization/statement of Medical Necessity/order Form
Get, Create, Make and Sign new mexico prior authorizationstatement



How to edit new mexico prior authorizationstatement online
Uncompromising security for your PDF editing and eSignature needs
How to fill out new mexico prior authorizationstatement

How to fill out new mexico prior authorizationstatement
Who needs new mexico prior authorizationstatement?
New Mexico prior authorization statement form: A comprehensive guide
Understanding prior authorization in New Mexico
Prior authorization is a crucial process in healthcare that requires providers to obtain approval from an insurer before performing certain services or prescribing specific medications. This ensures that the treatment is necessary, appropriate, and covered under the patient's health plan.
In New Mexico, prior authorization serves as a gatekeeper to manage healthcare costs and prevent unnecessary expenses. It plays an essential role in ensuring that providers deliver care that aligns with the latest evidence-based guidelines, which ultimately protects patient safety and health outcomes.
New Mexico's prior authorization regulations are crafted to provide a streamlined process while balancing the needs of patients and providers. They stipulate clear guidelines for what requires authorization and the timeframe for responses from insurers.
Who needs to use the New Mexico prior authorization statement form?
The New Mexico prior authorization statement form is essential for specific individuals and entities. Patients who require certain medical treatments or medications dictated by their insurance policies typically need to have this form completed. This form is also crucial for healthcare providers who must ensure that the services they are providing will be reimbursed by the patient's insurance.
Insurance companies implement prior authorization policies to manage costs and ensure that patients receive appropriate care. Therefore, understanding these requirements is vital for anyone navigating the healthcare system in New Mexico.
Key components of the New Mexico prior authorization statement form
The New Mexico prior authorization statement form contains specific sections that are critical for proper submission. Below are the key components that require thorough attention:
Step-by-step guide to completing the form
Completing the New Mexico prior authorization statement form need not be complicated if you follow these organized steps:
Managing your prior authorization requests
Once the prior authorization request is submitted, tracking its status becomes crucial. Insurers are required to respond within a specific timeframe. If your request is denied, understanding the reason behind the denial can help address any issues.
Engaging in effective communication with both your provider and insurer can enhance your chances of success. Here’s what you can do if your request is denied:
Frequently asked questions (FAQs) about New Mexico prior authorization
Patients and providers often have common questions about the New Mexico prior authorization statement form. Here are answers to some frequently asked questions:
Interactive tools for easy document management
Utilizing digital tools can significantly simplify the process of managing prior authorization requests. pdfFiller offers powerful features that enhance your ability to complete, submit, and track your forms effectively.
Stay updated on changes and news related to prior authorization in New Mexico
The landscape of healthcare and prior authorization is continually evolving. It is important to stay informed about any legislative changes that may impact the process.
Utilizing technology for a smoother prior authorization experience
Adopting cloud-based document solutions, like those offered by pdfFiller, can greatly enhance your prior authorization experience. Here are several benefits of using such technology:






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit new mexico prior authorizationstatement straight from my smartphone?
How do I complete new mexico prior authorizationstatement on an iOS device?
Can I edit new mexico prior authorizationstatement on an Android device?
What is new mexico prior authorization statement?
Who is required to file new mexico prior authorization statement?
How to fill out new mexico prior authorization statement?
What is the purpose of new mexico prior authorization statement?
What information must be reported on new mexico prior authorization statement?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.